Aldosteronism
Published: 18 Jun 2025
ICD9: 255.10 ICD10: E26.9 ICD11: 5A72.0
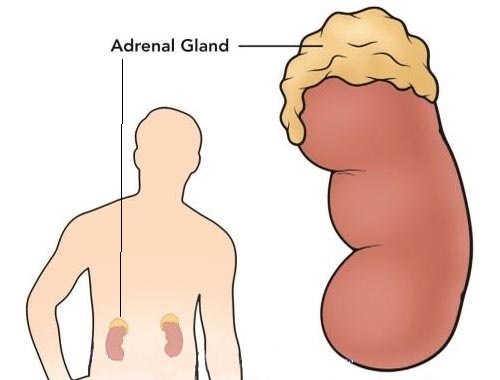
Aldosteronism, also known as hyperaldosteronism, is a condition in which the adrenal glands produce too much aldosterone.
Aldosterone is a hormone that helps regulate blood pressure and the balance of sodium and potassium in the blood.
Here's a more detailed breakdown:
![]() Aldosterone's Role: Aldosterone acts primarily on the kidneys, signaling them to retain sodium and excrete potassium. This helps maintain blood volume and, consequently, blood pressure.
Aldosterone's Role: Aldosterone acts primarily on the kidneys, signaling them to retain sodium and excrete potassium. This helps maintain blood volume and, consequently, blood pressure.
![]() What Happens in Aldosteronism: When there's too much aldosterone, the kidneys retain excessive amounts of sodium, leading to:
What Happens in Aldosteronism: When there's too much aldosterone, the kidneys retain excessive amounts of sodium, leading to:![]()

![]() High blood pressure (hypertension): The excess sodium causes increased fluid retention, raising blood volume and pressure.
High blood pressure (hypertension): The excess sodium causes increased fluid retention, raising blood volume and pressure.![]()

![]() Low potassium levels (hypokalemia): The kidneys excrete too much potassium, leading to this imbalance. Hypokalemia can cause muscle weakness, fatigue, cramps, and, in severe cases, heart rhythm problems.
Low potassium levels (hypokalemia): The kidneys excrete too much potassium, leading to this imbalance. Hypokalemia can cause muscle weakness, fatigue, cramps, and, in severe cases, heart rhythm problems.
![]() Types of Aldosteronism:
Types of Aldosteronism:![]()

![]() Primary Aldosteronism (Conn's Syndrome): The problem originates within the adrenal glands themselves. Common causes include:
Primary Aldosteronism (Conn's Syndrome): The problem originates within the adrenal glands themselves. Common causes include:![]()

![]() Adrenal adenoma (a non-cancerous tumor): This is the most frequent cause. The tumor produces aldosterone autonomously, without the normal regulatory signals.
Adrenal adenoma (a non-cancerous tumor): This is the most frequent cause. The tumor produces aldosterone autonomously, without the normal regulatory signals.![]()

![]() Bilateral adrenal hyperplasia: Both adrenal glands are enlarged and overactive.
Bilateral adrenal hyperplasia: Both adrenal glands are enlarged and overactive.![]()

![]() Rarely, adrenal carcinoma (cancer).
Rarely, adrenal carcinoma (cancer).![]()

![]() Familial hyperaldosteronism: A genetic condition causing increased aldosterone production.
Familial hyperaldosteronism: A genetic condition causing increased aldosterone production.![]()

![]() Secondary Aldosteronism: The excessive aldosterone production is triggered by a problem outside of the adrenal glands. This is usually the body's response to:
Secondary Aldosteronism: The excessive aldosterone production is triggered by a problem outside of the adrenal glands. This is usually the body's response to:![]()

![]() Reduced blood flow to the kidneys: Conditions like renal artery stenosis (narrowing of the arteries to the kidneys) or heart failure can reduce blood flow. The kidneys mistakenly interpret this as low blood volume and release renin, which ultimately stimulates aldosterone production.
Reduced blood flow to the kidneys: Conditions like renal artery stenosis (narrowing of the arteries to the kidneys) or heart failure can reduce blood flow. The kidneys mistakenly interpret this as low blood volume and release renin, which ultimately stimulates aldosterone production.![]()

![]() Sodium depletion: Severe sodium loss (e.g., through diuretics or excessive sweating) can trigger the renin-angiotensin-aldosterone system (RAAS), leading to increased aldosterone.
Sodium depletion: Severe sodium loss (e.g., through diuretics or excessive sweating) can trigger the renin-angiotensin-aldosterone system (RAAS), leading to increased aldosterone.![]()

![]() Dehydration: Similar to sodium depletion, dehydration can activate RAAS.
Dehydration: Similar to sodium depletion, dehydration can activate RAAS.![]()

![]() Cirrhosis (liver disease): Can lead to fluid retention and secondary aldosteronism.
Cirrhosis (liver disease): Can lead to fluid retention and secondary aldosteronism.![]()

![]() Nephrotic syndrome (kidney disease): Can cause sodium retention.
Nephrotic syndrome (kidney disease): Can cause sodium retention.
![]() Symptoms:
Symptoms:![]()

![]() Hypertension (often difficult to control)
Hypertension (often difficult to control)![]()

![]() Fatigue
Fatigue![]()

![]() Muscle weakness
Muscle weakness![]()

![]() Muscle cramps or spasms
Muscle cramps or spasms![]()

![]() Headache
Headache![]()

![]() Increased thirst
Increased thirst![]()

![]() Frequent urination, especially at night (nocturia)
Frequent urination, especially at night (nocturia)![]()

![]() Palpitations (irregular heartbeats) - due to low potassium
Palpitations (irregular heartbeats) - due to low potassium![]()

![]() In some cases, there may be no noticeable symptoms.
In some cases, there may be no noticeable symptoms.
![]() Diagnosis:
Diagnosis:![]()

![]() Blood tests: To measure aldosterone, renin, sodium, and potassium levels.
Blood tests: To measure aldosterone, renin, sodium, and potassium levels.![]()

![]() Urine tests: To measure aldosterone levels.
Urine tests: To measure aldosterone levels.![]()

![]() Aldosterone suppression test: Involves administering saline solution (salt water) or a medication to suppress aldosterone production. If aldosterone levels remain high despite suppression, it suggests primary aldosteronism.
Aldosterone suppression test: Involves administering saline solution (salt water) or a medication to suppress aldosterone production. If aldosterone levels remain high despite suppression, it suggests primary aldosteronism.![]()

![]() Adrenal imaging (CT scan or MRI): To look for adrenal adenomas or hyperplasia.
Adrenal imaging (CT scan or MRI): To look for adrenal adenomas or hyperplasia.![]()

![]() Adrenal vein sampling (AVS): A more invasive procedure where blood samples are taken directly from the veins draining each adrenal gland. This can help determine if the aldosterone is coming from one gland (suggesting an adenoma) or both glands (suggesting hyperplasia).
Adrenal vein sampling (AVS): A more invasive procedure where blood samples are taken directly from the veins draining each adrenal gland. This can help determine if the aldosterone is coming from one gland (suggesting an adenoma) or both glands (suggesting hyperplasia).
![]() Treatment:
Treatment:![]()

![]() Primary aldosteronism:
Primary aldosteronism:![]()

![]() Surgery (adrenalectomy): For adrenal adenomas, surgical removal of the affected adrenal gland is often the best option.
Surgery (adrenalectomy): For adrenal adenomas, surgical removal of the affected adrenal gland is often the best option.![]()

![]() Medications:
Medications:
* Mineralocorticoid receptor antagonists (e.g., spironolactone, eplerenone): These drugs block the effects of aldosterone. They are used for bilateral adrenal hyperplasia or when surgery is not an option.
* Blood pressure medications: To control hypertension.![]()

![]() Secondary aldosteronism: Treatment focuses on addressing the underlying cause. For example, treating renal artery stenosis or managing heart failure.
Secondary aldosteronism: Treatment focuses on addressing the underlying cause. For example, treating renal artery stenosis or managing heart failure.
It's important to consult a doctor if you suspect you have aldosteronism. Early diagnosis and treatment can help prevent serious complications.