Alzheimer’s Disease
Published: 18 Jun 2025
ICD9: 331.0 ICD10: G30.9 ICD11: 6D80.3
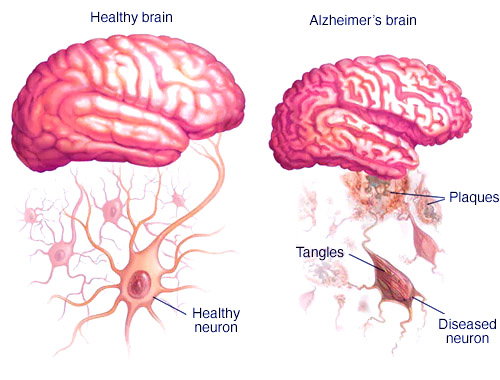
Alzheimer's disease is a progressive neurodegenerative disease that gradually destroys memory and thinking skills, and eventually the ability to carry out the simplest tasks.
It is the most common cause of dementia, a general term for a decline in mental ability severe enough to interfere with daily life.
Here's a breakdown of key aspects of Alzheimer's disease:
Core Features:
![]() Progressive: The disease worsens over time, with symptoms gradually increasing in severity.
Progressive: The disease worsens over time, with symptoms gradually increasing in severity.
![]() Neurodegenerative: It involves the degeneration and death of brain cells, particularly in regions involved in memory, learning, and cognition.
Neurodegenerative: It involves the degeneration and death of brain cells, particularly in regions involved in memory, learning, and cognition.
![]() Dementia: Alzheimer's is a type of dementia, but not all dementia is Alzheimer's.
Dementia: Alzheimer's is a type of dementia, but not all dementia is Alzheimer's.
Symptoms:
The symptoms of Alzheimer's disease vary from person to person and depend on the stage of the disease. Common symptoms include:
![]() Memory Loss: Difficulty remembering newly learned information, dates, events, and repeatedly asking the same questions. This is often one of the earliest and most noticeable signs.
Memory Loss: Difficulty remembering newly learned information, dates, events, and repeatedly asking the same questions. This is often one of the earliest and most noticeable signs.
![]() Cognitive Decline:
Cognitive Decline:![]()

![]() Difficulty with planning or problem-solving.
Difficulty with planning or problem-solving.![]()

![]() Trouble with familiar tasks at home, at work, or during leisure activities.
Trouble with familiar tasks at home, at work, or during leisure activities.![]()

![]() Confusion with time or place.
Confusion with time or place.![]()

![]() Difficulty understanding visual images and spatial relationships.
Difficulty understanding visual images and spatial relationships.![]()

![]() Problems with words in speaking or writing.
Problems with words in speaking or writing.![]()

![]() Misplacing things and losing the ability to retrace steps.
Misplacing things and losing the ability to retrace steps.![]()

![]() Decreased or poor judgment.
Decreased or poor judgment.
![]() Changes in Mood and Personality:
Changes in Mood and Personality:![]()

![]() Depression
Depression![]()

![]() Anxiety
Anxiety![]()

![]() Irritability and mood swings
Irritability and mood swings![]()

![]() Aggression
Aggression![]()

![]() Social withdrawal
Social withdrawal![]()

![]() Changes in sleep habits
Changes in sleep habits![]()

![]() Wandering
Wandering
![]() Later Stages: In the later stages, individuals may have difficulty speaking, swallowing, and walking. They may become completely dependent on others for care.
Later Stages: In the later stages, individuals may have difficulty speaking, swallowing, and walking. They may become completely dependent on others for care.
Causes:
The exact causes of Alzheimer's disease are not fully understood, but research suggests that it develops from a complex combination of genetic, lifestyle, and environmental factors.
![]() Plaques and Tangles: Two abnormal protein structures, amyloid plaques and neurofibrillary tangles (made of tau protein), are considered hallmarks of Alzheimer's disease in the brain. These are thought to interfere with communication between brain cells and disrupt cell function.
Plaques and Tangles: Two abnormal protein structures, amyloid plaques and neurofibrillary tangles (made of tau protein), are considered hallmarks of Alzheimer's disease in the brain. These are thought to interfere with communication between brain cells and disrupt cell function.
![]() Genetic Factors: While most cases are sporadic (not directly inherited), some genes increase the risk of developing Alzheimer's. Rare forms of Alzheimer's are directly caused by genetic mutations.
Genetic Factors: While most cases are sporadic (not directly inherited), some genes increase the risk of developing Alzheimer's. Rare forms of Alzheimer's are directly caused by genetic mutations.
![]() Age: The greatest known risk factor is increasing age. Most people with Alzheimer's are diagnosed after age 65.
Age: The greatest known risk factor is increasing age. Most people with Alzheimer's are diagnosed after age 65.
![]() Other Risk Factors:
Other Risk Factors:![]()

![]() Family history
Family history![]()

![]() Head injuries
Head injuries![]()

![]() Cardiovascular disease (heart disease, stroke, high blood pressure, high cholesterol)
Cardiovascular disease (heart disease, stroke, high blood pressure, high cholesterol)![]()

![]() Lifestyle factors (lack of exercise, poor diet, smoking)
Lifestyle factors (lack of exercise, poor diet, smoking)
Diagnosis:
Diagnosing Alzheimer's disease involves a comprehensive evaluation that includes:
![]() Medical History and Physical Exam: To assess overall health and identify other possible causes of symptoms.
Medical History and Physical Exam: To assess overall health and identify other possible causes of symptoms.
![]() Cognitive and Neurological Tests: To evaluate memory, thinking skills, language abilities, and motor skills. These might include the Mini-Mental State Examination (MMSE) or the Montreal Cognitive Assessment (MoCA).
Cognitive and Neurological Tests: To evaluate memory, thinking skills, language abilities, and motor skills. These might include the Mini-Mental State Examination (MMSE) or the Montreal Cognitive Assessment (MoCA).
![]() Brain Imaging: MRI or CT scans to look for structural changes in the brain, such as shrinkage or abnormalities. PET scans can sometimes be used to detect amyloid plaques and tau tangles.
Brain Imaging: MRI or CT scans to look for structural changes in the brain, such as shrinkage or abnormalities. PET scans can sometimes be used to detect amyloid plaques and tau tangles.
![]() Blood Tests: To rule out other medical conditions that could be causing similar symptoms.
Blood Tests: To rule out other medical conditions that could be causing similar symptoms.
Treatment:
There is currently no cure for Alzheimer's disease, but treatments are available to manage symptoms and potentially slow down the progression of the disease in some people.
![]() Medications:
Medications:![]()

![]() Cholinesterase inhibitors (e.g., donepezil, rivastigmine, galantamine): These medications can help improve cognitive function by increasing levels of a neurotransmitter called acetylcholine.
Cholinesterase inhibitors (e.g., donepezil, rivastigmine, galantamine): These medications can help improve cognitive function by increasing levels of a neurotransmitter called acetylcholine.![]()

![]() Memantine: This medication regulates the activity of glutamate, another neurotransmitter, and can help with memory and thinking problems.
Memantine: This medication regulates the activity of glutamate, another neurotransmitter, and can help with memory and thinking problems.![]()

![]() Aducanumab and Lecanemab: These are newer monoclonal antibody medications that target amyloid plaques in the brain. They have shown some promise in slowing the progression of the disease in early stages, but they also have potential side effects and are not suitable for everyone.
Aducanumab and Lecanemab: These are newer monoclonal antibody medications that target amyloid plaques in the brain. They have shown some promise in slowing the progression of the disease in early stages, but they also have potential side effects and are not suitable for everyone.
![]() Non-pharmacological Interventions:
Non-pharmacological Interventions:![]()

![]() Cognitive therapies: Like memory training and reality orientation.
Cognitive therapies: Like memory training and reality orientation.![]()

![]() Behavioral therapies: To manage agitation, anxiety, and other behavioral problems.
Behavioral therapies: To manage agitation, anxiety, and other behavioral problems.![]()

![]() Support groups: For individuals with Alzheimer's and their caregivers.
Support groups: For individuals with Alzheimer's and their caregivers.![]()

![]() Lifestyle modifications: Including a healthy diet, regular exercise, social engagement, and mental stimulation.
Lifestyle modifications: Including a healthy diet, regular exercise, social engagement, and mental stimulation.
Prevention:
While there is no guaranteed way to prevent Alzheimer's disease, research suggests that certain lifestyle factors may reduce the risk:
![]() Heart-healthy lifestyle: Maintaining a healthy weight, controlling blood pressure and cholesterol, and not smoking.
Heart-healthy lifestyle: Maintaining a healthy weight, controlling blood pressure and cholesterol, and not smoking.
![]() Regular exercise: Both physical and mental exercise can help protect the brain.
Regular exercise: Both physical and mental exercise can help protect the brain.
![]() Healthy diet: A diet rich in fruits, vegetables, and whole grains. The Mediterranean diet is often recommended.
Healthy diet: A diet rich in fruits, vegetables, and whole grains. The Mediterranean diet is often recommended.
![]() Mental stimulation: Engaging in activities that challenge the brain, such as reading, puzzles, and learning new skills.
Mental stimulation: Engaging in activities that challenge the brain, such as reading, puzzles, and learning new skills.
![]() Social engagement: Staying connected with friends and family.
Social engagement: Staying connected with friends and family.
Impact:
Alzheimer's disease has a profound impact on individuals, families, and society. It can lead to:
![]() Loss of independence: As the disease progresses, individuals may need assistance with daily tasks.
Loss of independence: As the disease progresses, individuals may need assistance with daily tasks.
![]() Emotional distress: For both the person with Alzheimer's and their caregivers.
Emotional distress: For both the person with Alzheimer's and their caregivers.
![]() Financial burden: Due to the cost of care and treatment.
Financial burden: Due to the cost of care and treatment.
![]() Significant caregiver burden: Caregivers often experience high levels of stress, depression, and burnout.
Significant caregiver burden: Caregivers often experience high levels of stress, depression, and burnout.
In summary, Alzheimer's disease is a devastating illness that slowly robs people of their memories, cognitive abilities, and ultimately, their independence. While there is no cure, early diagnosis and treatment can help manage symptoms and potentially slow the progression of the disease. Research continues to advance our understanding of Alzheimer's, and there is hope for new and more effective treatments in the future.