Androgenic alopecia (Hair Loss)
Published: 18 Jun 2025
ICD9: 704.09 ICD10: L66.8 ICD11: ED70
Androgenic alopecia, commonly known as male-pattern baldness or female-pattern baldness, is a common type of hair loss that affects both men and women.
It's a gradual process driven by a combination of genetic predisposition and hormonal influences, specifically the androgen hormone dihydrotestosterone (DHT).
Here's a breakdown of what it is:
![]() Genetic Predisposition: The likelihood of developing androgenic alopecia is heavily influenced by your genes. You inherit a tendency for hair follicles to be more sensitive to the effects of DHT.
Genetic Predisposition: The likelihood of developing androgenic alopecia is heavily influenced by your genes. You inherit a tendency for hair follicles to be more sensitive to the effects of DHT.
![]() Hormonal Influence (DHT): The enzyme 5-alpha-reductase converts testosterone (a male sex hormone, present in both men and women) into DHT. DHT binds to receptors in hair follicles, causing them to shrink (miniaturization). Over time, these miniaturized follicles produce thinner, shorter, and less pigmented hairs. Eventually, they may stop producing hair altogether.
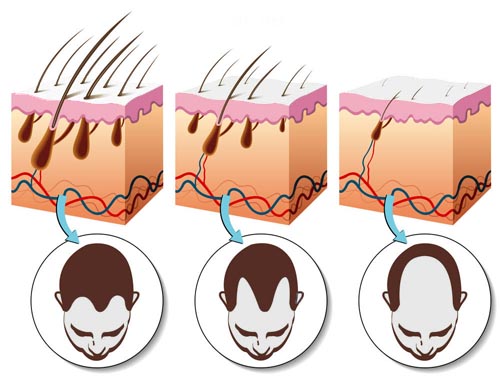
Hormonal Influence (DHT): The enzyme 5-alpha-reductase converts testosterone (a male sex hormone, present in both men and women) into DHT. DHT binds to receptors in hair follicles, causing them to shrink (miniaturization). Over time, these miniaturized follicles produce thinner, shorter, and less pigmented hairs. Eventually, they may stop producing hair altogether.
![]() Patterned Hair Loss: The hair loss follows a characteristic pattern.
Patterned Hair Loss: The hair loss follows a characteristic pattern.![]()

![]() Men: Typically begins with a receding hairline (often an "M" shape) and/or thinning at the crown of the head. It can progress to complete or near-complete baldness.
Men: Typically begins with a receding hairline (often an "M" shape) and/or thinning at the crown of the head. It can progress to complete or near-complete baldness.![]()

![]() Women: Usually presents as a more diffuse thinning over the top of the head, with the frontal hairline generally remaining intact. The Ludwig scale is often used to classify the severity.
Women: Usually presents as a more diffuse thinning over the top of the head, with the frontal hairline generally remaining intact. The Ludwig scale is often used to classify the severity.
![]() Key Characteristics:
Key Characteristics:![]()

![]() Gradual Onset: The hair loss is typically a slow and progressive process that can take years or decades.
Gradual Onset: The hair loss is typically a slow and progressive process that can take years or decades.![]()

![]() Miniaturization: A hallmark of androgenic alopecia is the miniaturization of hair follicles. Hair becomes thinner and shorter.
Miniaturization: A hallmark of androgenic alopecia is the miniaturization of hair follicles. Hair becomes thinner and shorter.![]()

![]() Non-Scarring: Androgenic alopecia is a non-scarring type of hair loss. The hair follicles are still present (though miniaturized) and potentially can be stimulated to grow.
Non-Scarring: Androgenic alopecia is a non-scarring type of hair loss. The hair follicles are still present (though miniaturized) and potentially can be stimulated to grow.
![]() Differences in Men and Women:
Differences in Men and Women:![]()

![]() While the underlying mechanisms are similar, the presentation and hormonal aspects can differ between men and women. Women may experience androgenic alopecia in association with conditions like polycystic ovary syndrome (PCOS), which can lead to elevated androgen levels.
While the underlying mechanisms are similar, the presentation and hormonal aspects can differ between men and women. Women may experience androgenic alopecia in association with conditions like polycystic ovary syndrome (PCOS), which can lead to elevated androgen levels.![]()

![]() Treatment options may also vary depending on sex.
Treatment options may also vary depending on sex.
![]() Diagnosis: A doctor or dermatologist can diagnose androgenic alopecia based on the pattern of hair loss, medical history, and sometimes by examining the scalp with a dermatoscope (a magnifying device). In some cases, blood tests might be done to rule out other causes of hair loss. A scalp biopsy may be considered in atypical cases.
Diagnosis: A doctor or dermatologist can diagnose androgenic alopecia based on the pattern of hair loss, medical history, and sometimes by examining the scalp with a dermatoscope (a magnifying device). In some cases, blood tests might be done to rule out other causes of hair loss. A scalp biopsy may be considered in atypical cases.
![]() Treatment: Treatment options aim to slow down hair loss, stimulate hair regrowth, or cover up the bald areas. Common treatments include:
Treatment: Treatment options aim to slow down hair loss, stimulate hair regrowth, or cover up the bald areas. Common treatments include:![]()

![]() Minoxidil (Rogaine): A topical medication that stimulates hair growth and slows down hair loss. It's available over-the-counter.
Minoxidil (Rogaine): A topical medication that stimulates hair growth and slows down hair loss. It's available over-the-counter.![]()

![]() Finasteride (Propecia): An oral medication (prescription only) that blocks the production of DHT. It's generally used for men. Women of childbearing potential should not take Finasteride.
Finasteride (Propecia): An oral medication (prescription only) that blocks the production of DHT. It's generally used for men. Women of childbearing potential should not take Finasteride.![]()

![]() Spironolactone: An oral medication (prescription only) that is sometimes used off-label in women to block androgen receptors.
Spironolactone: An oral medication (prescription only) that is sometimes used off-label in women to block androgen receptors.![]()

![]() Low-Level Laser Therapy (LLLT): Devices like laser combs or helmets are used to stimulate hair follicles.
Low-Level Laser Therapy (LLLT): Devices like laser combs or helmets are used to stimulate hair follicles.![]()

![]() Hair Transplantation: Surgical procedure where hair follicles are transplanted from areas of the scalp with healthy hair growth to bald or thinning areas.
Hair Transplantation: Surgical procedure where hair follicles are transplanted from areas of the scalp with healthy hair growth to bald or thinning areas.![]()

![]() Platelet-Rich Plasma (PRP) Therapy: Involves injecting concentrated platelets from the patient's own blood into the scalp to stimulate hair growth.
Platelet-Rich Plasma (PRP) Therapy: Involves injecting concentrated platelets from the patient's own blood into the scalp to stimulate hair growth.![]()

![]() Other Options: Wigs, hairpieces, and scalp micropigmentation can provide cosmetic solutions.
Other Options: Wigs, hairpieces, and scalp micropigmentation can provide cosmetic solutions.
It's important to consult with a doctor or dermatologist to determine the underlying cause of your hair loss and discuss the most appropriate treatment options for you.