Anovulation
Published: 18 Jun 2025
ICD9: 628.0 ICD10: N97.0 ICD11: 5A80.3
Anovulation is the absence of ovulation, meaning that the ovary doesn't release an egg during a menstrual cycle.
It's a common cause of infertility, but it's also something that can happen occasionally to women who are otherwise fertile.
Here's a breakdown:
![]() Ovulation: This is the process where a mature egg is released from the ovary and travels down the fallopian tube, ready to be fertilized by sperm. It's a crucial step in the female reproductive cycle.
Ovulation: This is the process where a mature egg is released from the ovary and travels down the fallopian tube, ready to be fertilized by sperm. It's a crucial step in the female reproductive cycle.
![]() Anovulation: When ovulation doesn't occur during a menstrual cycle, it's called anovulation. This means there's no egg available to be fertilized, making pregnancy impossible during that cycle.
Anovulation: When ovulation doesn't occur during a menstrual cycle, it's called anovulation. This means there's no egg available to be fertilized, making pregnancy impossible during that cycle.
Causes of Anovulation:
Anovulation can be caused by a variety of factors, including:
![]() Hormonal imbalances: This is one of the most common causes. Problems with the hormones that regulate the menstrual cycle (such as follicle-stimulating hormone (FSH), luteinizing hormone (LH), estrogen, and progesterone) can disrupt ovulation. Conditions like Polycystic Ovary Syndrome (PCOS) are a frequent culprit.
Hormonal imbalances: This is one of the most common causes. Problems with the hormones that regulate the menstrual cycle (such as follicle-stimulating hormone (FSH), luteinizing hormone (LH), estrogen, and progesterone) can disrupt ovulation. Conditions like Polycystic Ovary Syndrome (PCOS) are a frequent culprit.
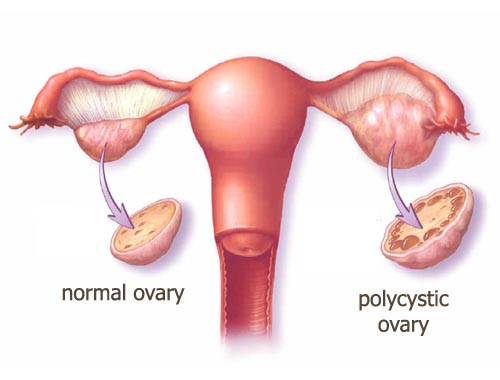
![]() Polycystic Ovary Syndrome (PCOS): A hormonal disorder common among women of reproductive age. It's characterized by infrequent or prolonged menstrual periods or excess male hormone (androgen) levels. PCOS is a major cause of anovulation.
Polycystic Ovary Syndrome (PCOS): A hormonal disorder common among women of reproductive age. It's characterized by infrequent or prolonged menstrual periods or excess male hormone (androgen) levels. PCOS is a major cause of anovulation.
![]() Weight issues: Being significantly underweight or overweight can affect hormone production and disrupt ovulation. Eating disorders like anorexia and bulimia can also cause anovulation.
Weight issues: Being significantly underweight or overweight can affect hormone production and disrupt ovulation. Eating disorders like anorexia and bulimia can also cause anovulation.
![]() Stress: High levels of stress can interfere with the hormones that control ovulation.
Stress: High levels of stress can interfere with the hormones that control ovulation.
![]() Thyroid problems: Both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can affect ovulation.
Thyroid problems: Both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can affect ovulation.
![]() Premature ovarian failure (POF): Also known as primary ovarian insufficiency, this is when the ovaries stop working normally before age 40.
Premature ovarian failure (POF): Also known as primary ovarian insufficiency, this is when the ovaries stop working normally before age 40.
![]() Certain medications: Some medications, such as antidepressants, antipsychotics, and corticosteroids, can interfere with ovulation.
Certain medications: Some medications, such as antidepressants, antipsychotics, and corticosteroids, can interfere with ovulation.
![]() Breastfeeding: Breastfeeding can suppress ovulation, especially in the early months after childbirth.
Breastfeeding: Breastfeeding can suppress ovulation, especially in the early months after childbirth.
![]() Perimenopause: As women approach menopause, their menstrual cycles become less regular, and they may experience anovulatory cycles more frequently.
Perimenopause: As women approach menopause, their menstrual cycles become less regular, and they may experience anovulatory cycles more frequently.
![]() Excessive exercise: Intense physical activity, especially when coupled with low body fat, can sometimes disrupt ovulation.
Excessive exercise: Intense physical activity, especially when coupled with low body fat, can sometimes disrupt ovulation.
![]() Pituitary gland disorders: The pituitary gland produces hormones that regulate ovulation. Problems with the pituitary gland can cause anovulation.
Pituitary gland disorders: The pituitary gland produces hormones that regulate ovulation. Problems with the pituitary gland can cause anovulation.
Symptoms of Anovulation:
![]() Irregular periods: Periods may be infrequent, very long, very short, or absent altogether.
Irregular periods: Periods may be infrequent, very long, very short, or absent altogether.
![]() Absent periods (amenorrhea): No menstruation at all.
Absent periods (amenorrhea): No menstruation at all.
![]() Unusually light or heavy bleeding: Changes in the amount or duration of bleeding during periods.
Unusually light or heavy bleeding: Changes in the amount or duration of bleeding during periods.
![]() Lack of premenstrual symptoms (PMS): Symptoms like breast tenderness, bloating, and mood changes that typically occur before menstruation may be absent.
Lack of premenstrual symptoms (PMS): Symptoms like breast tenderness, bloating, and mood changes that typically occur before menstruation may be absent.
![]() Difficulty getting pregnant (infertility): This is often the primary way anovulation is discovered.
Difficulty getting pregnant (infertility): This is often the primary way anovulation is discovered.
![]() No change in basal body temperature (BBT): Typically, BBT rises slightly after ovulation. If ovulation isn't occurring, there won't be a noticeable temperature shift.
No change in basal body temperature (BBT): Typically, BBT rises slightly after ovulation. If ovulation isn't occurring, there won't be a noticeable temperature shift.
![]() Lack of cervical mucus changes: Cervical mucus usually becomes clear and stretchy around the time of ovulation. If ovulation isn't occurring, these changes may not be present.
Lack of cervical mucus changes: Cervical mucus usually becomes clear and stretchy around the time of ovulation. If ovulation isn't occurring, these changes may not be present.
![]() Negative ovulation predictor kits (OPKs): These kits detect the surge in LH that precedes ovulation. If ovulation isn't occurring, the kits will consistently show negative results.
Negative ovulation predictor kits (OPKs): These kits detect the surge in LH that precedes ovulation. If ovulation isn't occurring, the kits will consistently show negative results.
Diagnosis:
A doctor can diagnose anovulation based on:
![]() Medical history and physical exam: Discussing menstrual cycles, medical conditions, and lifestyle factors.
Medical history and physical exam: Discussing menstrual cycles, medical conditions, and lifestyle factors.
![]() Blood tests: To check hormone levels (FSH, LH, estrogen, progesterone, thyroid hormones, prolactin). Progesterone levels are often checked about a week before an expected period to see if ovulation occurred.
Blood tests: To check hormone levels (FSH, LH, estrogen, progesterone, thyroid hormones, prolactin). Progesterone levels are often checked about a week before an expected period to see if ovulation occurred.
![]() Ultrasound: To examine the ovaries and uterus.
Ultrasound: To examine the ovaries and uterus.
![]() Endometrial biopsy: In some cases, a small sample of the uterine lining may be taken to evaluate the effects of hormones on the uterus.
Endometrial biopsy: In some cases, a small sample of the uterine lining may be taken to evaluate the effects of hormones on the uterus.
Treatment:
Treatment for anovulation depends on the underlying cause and the woman's goals (e.g., pregnancy or simply regulating periods). Options may include:
![]() Lifestyle changes: Weight management, stress reduction, and dietary adjustments can sometimes help regulate ovulation.
Lifestyle changes: Weight management, stress reduction, and dietary adjustments can sometimes help regulate ovulation.
![]() Medications:
Medications:![]()

![]() Clomiphene citrate (Clomid): A medication that stimulates the ovaries to release an egg.
Clomiphene citrate (Clomid): A medication that stimulates the ovaries to release an egg.![]()

![]() Letrozole (Femara): Another medication used to induce ovulation.
Letrozole (Femara): Another medication used to induce ovulation.![]()

![]() Metformin: Often used to treat PCOS, it can help regulate insulin levels and improve ovulation.
Metformin: Often used to treat PCOS, it can help regulate insulin levels and improve ovulation.![]()

![]() Gonadotropins (FSH and LH injections): Powerful hormones that directly stimulate the ovaries.
Gonadotropins (FSH and LH injections): Powerful hormones that directly stimulate the ovaries.
![]() Surgery: In rare cases, surgery may be necessary to correct underlying problems with the ovaries or other reproductive organs.
Surgery: In rare cases, surgery may be necessary to correct underlying problems with the ovaries or other reproductive organs.
![]() Treating underlying conditions: Addressing conditions like thyroid disorders or PCOS can often restore regular ovulation.
Treating underlying conditions: Addressing conditions like thyroid disorders or PCOS can often restore regular ovulation.
If a woman is trying to conceive, assisted reproductive technologies (ART) like in vitro fertilization (IVF) may be considered if other treatments are unsuccessful.
Important Considerations:
![]() Occasional anovulatory cycles are normal, especially around puberty, after pregnancy, and during perimenopause. It's not usually a cause for concern unless it becomes frequent or persistent.
Occasional anovulatory cycles are normal, especially around puberty, after pregnancy, and during perimenopause. It's not usually a cause for concern unless it becomes frequent or persistent.
![]() If you're concerned about irregular periods, difficulty getting pregnant, or other symptoms of anovulation, it's important to see a doctor for diagnosis and treatment. Early diagnosis and treatment can improve the chances of conception and address any underlying health issues.
If you're concerned about irregular periods, difficulty getting pregnant, or other symptoms of anovulation, it's important to see a doctor for diagnosis and treatment. Early diagnosis and treatment can improve the chances of conception and address any underlying health issues.
![]() If you are sexually active and do not wish to become pregnant, irregular cycles do not mean you can forgo contraception. Pregnancy is still possible, though less likely with anovulation.
If you are sexually active and do not wish to become pregnant, irregular cycles do not mean you can forgo contraception. Pregnancy is still possible, though less likely with anovulation.
In summary, anovulation is the absence of ovulation and a common cause of infertility. It can be caused by various factors, including hormonal imbalances, weight issues, stress, and underlying medical conditions. Diagnosis involves a medical history, physical exam, and blood tests. Treatment options include lifestyle changes, medications, and addressing underlying conditions.