Aortic Stenosis
Published: 18 Jun 2025
ICD9: 424.1 ICD10: I35.0 ICD11: BB70
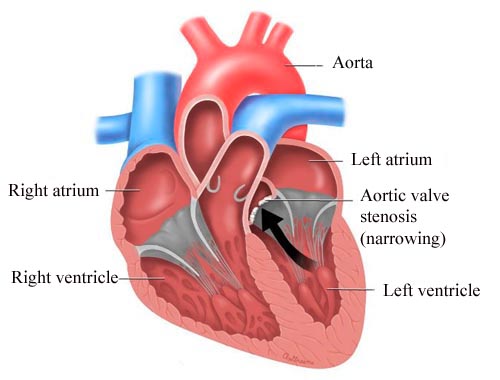
Aortic stenosis (AS) is a condition where the aortic valve narrows, restricting blood flow from the heart to the aorta and the rest of the body.
The aortic valve is the gateway between the left ventricle (the heart's main pumping chamber) and the aorta (the main artery that carries oxygen-rich blood away from the heart).
Think of it like this: Imagine a garden hose. If you pinch the hose (narrow the opening), less water can flow through. In aortic stenosis, the aortic valve acts like the pinched hose, making it harder for the heart to pump blood effectively.
Here's a breakdown of key aspects:
![]() Cause: The most common cause is age-related calcification (calcium deposits) of the valve. Other causes include:
Cause: The most common cause is age-related calcification (calcium deposits) of the valve. Other causes include:![]()

![]() Congenital valve defects: Being born with a malformed aortic valve (like a bicuspid valve instead of the normal tricuspid valve) can lead to stenosis later in life.
Congenital valve defects: Being born with a malformed aortic valve (like a bicuspid valve instead of the normal tricuspid valve) can lead to stenosis later in life.![]()

![]() Rheumatic fever: A complication of strep throat can damage the heart valves, including the aortic valve.
Rheumatic fever: A complication of strep throat can damage the heart valves, including the aortic valve.
![]() Mechanism: As the valve narrows, the left ventricle has to work harder to pump blood through the smaller opening. Over time, this extra workload can cause the left ventricle to thicken (hypertrophy). Eventually, the heart may become weakened and unable to pump enough blood to meet the body's needs, leading to heart failure.
Mechanism: As the valve narrows, the left ventricle has to work harder to pump blood through the smaller opening. Over time, this extra workload can cause the left ventricle to thicken (hypertrophy). Eventually, the heart may become weakened and unable to pump enough blood to meet the body's needs, leading to heart failure.
![]() Symptoms: Symptoms often develop gradually as the stenosis worsens. Some people may not experience any symptoms for years. Common symptoms include:
Symptoms: Symptoms often develop gradually as the stenosis worsens. Some people may not experience any symptoms for years. Common symptoms include:![]()

![]() Chest pain (angina): Especially with exertion.
Chest pain (angina): Especially with exertion.![]()

![]() Shortness of breath: Especially with exertion or when lying down.
Shortness of breath: Especially with exertion or when lying down.![]()

![]() Dizziness or lightheadedness: Especially with exertion.
Dizziness or lightheadedness: Especially with exertion.![]()

![]() Fainting (syncope): Especially with exertion.
Fainting (syncope): Especially with exertion.![]()

![]() Fatigue: Feeling tired or weak.
Fatigue: Feeling tired or weak.![]()

![]() Heart murmur: An abnormal sound heard through a stethoscope. This is often the first sign detected during a routine checkup.
Heart murmur: An abnormal sound heard through a stethoscope. This is often the first sign detected during a routine checkup.
![]() Diagnosis:
Diagnosis:![]()

![]() Physical exam: Listening to the heart with a stethoscope to detect a murmur.
Physical exam: Listening to the heart with a stethoscope to detect a murmur.![]()

![]() Echocardiogram (echo): An ultrasound of the heart to visualize the aortic valve and assess its function, as well as the size and function of the heart chambers. This is the primary diagnostic test.
Echocardiogram (echo): An ultrasound of the heart to visualize the aortic valve and assess its function, as well as the size and function of the heart chambers. This is the primary diagnostic test.![]()

![]() Electrocardiogram (ECG or EKG): To assess the heart's electrical activity and look for signs of heart strain.
Electrocardiogram (ECG or EKG): To assess the heart's electrical activity and look for signs of heart strain.![]()

![]() Chest X-ray: To look for an enlarged heart or fluid in the lungs.
Chest X-ray: To look for an enlarged heart or fluid in the lungs.![]()

![]() Cardiac catheterization: A more invasive procedure used to measure the pressure inside the heart chambers and assess the severity of the stenosis. Typically used when echocardiogram results are unclear or to assess for coronary artery disease at the same time.
Cardiac catheterization: A more invasive procedure used to measure the pressure inside the heart chambers and assess the severity of the stenosis. Typically used when echocardiogram results are unclear or to assess for coronary artery disease at the same time.![]()

![]() CT scan: Can be used to assess the amount of calcium on the aortic valve, helping to determine the severity of the stenosis.
CT scan: Can be used to assess the amount of calcium on the aortic valve, helping to determine the severity of the stenosis.
![]() Treatment: The treatment for aortic stenosis depends on the severity of the condition and the presence of symptoms.
Treatment: The treatment for aortic stenosis depends on the severity of the condition and the presence of symptoms.![]()

![]() Mild aortic stenosis: Often requires only regular monitoring with echocardiograms.
Mild aortic stenosis: Often requires only regular monitoring with echocardiograms.![]()

![]() Moderate aortic stenosis: May require more frequent monitoring and lifestyle changes (e.g., avoiding strenuous activity).
Moderate aortic stenosis: May require more frequent monitoring and lifestyle changes (e.g., avoiding strenuous activity).![]()

![]() Severe aortic stenosis: Typically requires valve replacement. The two main options are:
Severe aortic stenosis: Typically requires valve replacement. The two main options are:![]()

![]() Surgical aortic valve replacement (SAVR): Open-heart surgery to replace the damaged valve with a mechanical or biological valve.
Surgical aortic valve replacement (SAVR): Open-heart surgery to replace the damaged valve with a mechanical or biological valve.![]()

![]() Transcatheter aortic valve replacement (TAVR): A less invasive procedure where a new valve is inserted through a catheter (usually inserted in the groin) and guided to the heart. TAVR is now commonly used, especially in older or high-risk patients.
Transcatheter aortic valve replacement (TAVR): A less invasive procedure where a new valve is inserted through a catheter (usually inserted in the groin) and guided to the heart. TAVR is now commonly used, especially in older or high-risk patients.
![]() Complications: If left untreated, severe aortic stenosis can lead to serious complications, including:
Complications: If left untreated, severe aortic stenosis can lead to serious complications, including:![]()

![]() Heart failure
Heart failure![]()

![]() Arrhythmias (irregular heartbeats)
Arrhythmias (irregular heartbeats)![]()

![]() Sudden cardiac death
Sudden cardiac death
In summary, aortic stenosis is a serious condition that can restrict blood flow from the heart and lead to significant health problems. Early diagnosis and treatment are crucial to prevent complications and improve the quality of life. If you have symptoms suggestive of aortic stenosis, it's important to see a doctor for evaluation.