Bladder Cancer
Published: 18 Jun 2025
ICD9: 188.9 ICD10: C67.9 ICD11: 2C94
Bladder cancer is a type of cancer that begins in the cells lining the bladder.
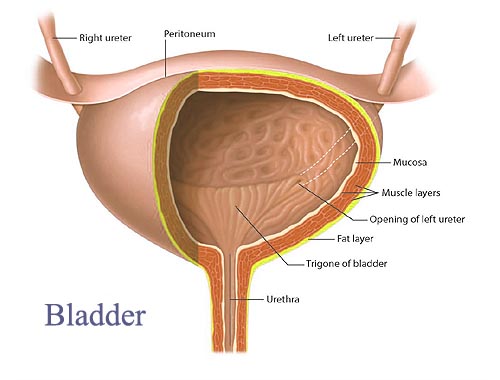
The bladder is a hollow, muscular organ in the lower abdomen that stores urine.
Here's a breakdown of key aspects of bladder cancer:
What it is:
![]() Cancer of the Bladder Lining: It most commonly starts in the urothelial cells (also known as transitional cells) that line the inside of the bladder. These same cells also line the kidneys, ureters (tubes that carry urine from the kidneys to the bladder), and urethra (the tube that carries urine from the bladder out of the body). Because of this, people who have bladder cancer have a slightly increased risk of developing cancers of these other organs.
Cancer of the Bladder Lining: It most commonly starts in the urothelial cells (also known as transitional cells) that line the inside of the bladder. These same cells also line the kidneys, ureters (tubes that carry urine from the kidneys to the bladder), and urethra (the tube that carries urine from the bladder out of the body). Because of this, people who have bladder cancer have a slightly increased risk of developing cancers of these other organs.
![]() Types:
Types:![]()

![]() Urothelial carcinoma (also called transitional cell carcinoma): This is the most common type (around 90% of bladder cancers).
Urothelial carcinoma (also called transitional cell carcinoma): This is the most common type (around 90% of bladder cancers).![]()

![]() Squamous cell carcinoma: A less common type, often linked to chronic irritation, such as from long-term catheter use or chronic bladder infections.
Squamous cell carcinoma: A less common type, often linked to chronic irritation, such as from long-term catheter use or chronic bladder infections.![]()

![]() Adenocarcinoma: A rare type, originating from gland-forming cells in the bladder.
Adenocarcinoma: A rare type, originating from gland-forming cells in the bladder.![]()

![]() Small cell carcinoma: A rare, aggressive type.
Small cell carcinoma: A rare, aggressive type.
Causes and Risk Factors:
While the exact cause isn't always clear, several factors increase the risk:
![]() Smoking: By far the biggest risk factor. Smokers are 3-4 times more likely to develop bladder cancer.
Smoking: By far the biggest risk factor. Smokers are 3-4 times more likely to develop bladder cancer.
![]() Age: The risk increases with age. Most people diagnosed are over 55.
Age: The risk increases with age. Most people diagnosed are over 55.
![]() Gender: Men are more likely to develop bladder cancer than women.
Gender: Men are more likely to develop bladder cancer than women.
![]() Race: White people are more likely to develop bladder cancer than African Americans.
Race: White people are more likely to develop bladder cancer than African Americans.
![]() Chemical Exposure: Certain chemicals used in dyes, rubber, leather, textiles, and paint products have been linked to bladder cancer. Workers in these industries are at higher risk.
Chemical Exposure: Certain chemicals used in dyes, rubber, leather, textiles, and paint products have been linked to bladder cancer. Workers in these industries are at higher risk.
![]() Chronic Bladder Irritation: Long-term bladder infections, kidney stones, or catheter use can increase the risk.
Chronic Bladder Irritation: Long-term bladder infections, kidney stones, or catheter use can increase the risk.
![]() Family History: Having a family history of bladder cancer increases your risk.
Family History: Having a family history of bladder cancer increases your risk.
![]() Previous Cancer Treatment: Certain chemotherapy drugs and radiation therapy to the pelvis can increase the risk.
Previous Cancer Treatment: Certain chemotherapy drugs and radiation therapy to the pelvis can increase the risk.
![]() Arsenic Exposure: Exposure to arsenic in drinking water.
Arsenic Exposure: Exposure to arsenic in drinking water.
![]() Certain Medications: Pioglitazone, a diabetes medication has been linked to an increased risk.
Certain Medications: Pioglitazone, a diabetes medication has been linked to an increased risk.
Symptoms:
![]() Blood in the urine (hematuria): This is the most common symptom. The urine may appear bright red or tea-colored. Sometimes, the blood is only detectable with a urine test.
Blood in the urine (hematuria): This is the most common symptom. The urine may appear bright red or tea-colored. Sometimes, the blood is only detectable with a urine test.
![]() Frequent urination: Feeling the need to urinate more often than usual.
Frequent urination: Feeling the need to urinate more often than usual.
![]() Painful urination (dysuria): Burning or pain when urinating.
Painful urination (dysuria): Burning or pain when urinating.
![]() Urgent need to urinate: A sudden, strong urge to urinate.
Urgent need to urinate: A sudden, strong urge to urinate.
![]() Lower back pain: This can occur if the cancer has spread.
Lower back pain: This can occur if the cancer has spread.
![]() Pelvic pain: This can occur if the cancer has spread.
Pelvic pain: This can occur if the cancer has spread.
Diagnosis:
![]() Physical Exam and History: The doctor will ask about your symptoms and medical history.
Physical Exam and History: The doctor will ask about your symptoms and medical history.
![]() Urinalysis: To check for blood, infection, and cancer cells in the urine.
Urinalysis: To check for blood, infection, and cancer cells in the urine.
![]() Urine Cytology: A test that examines urine samples under a microscope to look for abnormal cells.
Urine Cytology: A test that examines urine samples under a microscope to look for abnormal cells.
![]() Cystoscopy: A procedure where a thin, flexible tube with a camera (cystoscope) is inserted into the bladder through the urethra to visualize the bladder lining. Biopsies (tissue samples) can be taken during cystoscopy.
Cystoscopy: A procedure where a thin, flexible tube with a camera (cystoscope) is inserted into the bladder through the urethra to visualize the bladder lining. Biopsies (tissue samples) can be taken during cystoscopy.
![]() Biopsy: Removing a tissue sample for examination under a microscope to confirm the presence of cancer cells and determine the type and grade of cancer.
Biopsy: Removing a tissue sample for examination under a microscope to confirm the presence of cancer cells and determine the type and grade of cancer.
![]() Imaging Tests:
Imaging Tests:![]()

![]() CT scan (Computed Tomography): To create detailed images of the bladder, kidneys, ureters, and surrounding tissues.
CT scan (Computed Tomography): To create detailed images of the bladder, kidneys, ureters, and surrounding tissues.![]()

![]() MRI (Magnetic Resonance Imaging): Provides detailed images of the bladder and surrounding tissues.
MRI (Magnetic Resonance Imaging): Provides detailed images of the bladder and surrounding tissues.![]()

![]() Intravenous Pyelogram (IVP): X-rays of the urinary tract after injecting a dye.
Intravenous Pyelogram (IVP): X-rays of the urinary tract after injecting a dye.![]()

![]() Bone scan: To check if the cancer has spread to the bones.
Bone scan: To check if the cancer has spread to the bones.![]()

![]() Chest X-ray: To check if the cancer has spread to the lungs.
Chest X-ray: To check if the cancer has spread to the lungs.
Staging:
After diagnosis, the cancer is staged to determine the extent of its spread. Staging helps determine the best treatment options. Stages range from 0 to IV:
![]() Stage 0: Cancer is only in the inner lining of the bladder.
Stage 0: Cancer is only in the inner lining of the bladder.
![]() Stage I: Cancer has grown into the layer of tissue beneath the inner lining but has not reached the muscle layer.
Stage I: Cancer has grown into the layer of tissue beneath the inner lining but has not reached the muscle layer.
![]() Stage II: Cancer has grown into the muscle layer of the bladder.
Stage II: Cancer has grown into the muscle layer of the bladder.
![]() Stage III: Cancer has spread through the muscle layer to the surrounding tissue, and may have spread to the lymph nodes.
Stage III: Cancer has spread through the muscle layer to the surrounding tissue, and may have spread to the lymph nodes.
![]() Stage IV: Cancer has spread to distant sites, such as other organs (e.g., lungs, liver, bones) or distant lymph nodes.
Stage IV: Cancer has spread to distant sites, such as other organs (e.g., lungs, liver, bones) or distant lymph nodes.
Treatment:
Treatment options depend on the stage and grade of the cancer, as well as the person's overall health.
![]() Surgery:
Surgery:![]()

![]() Transurethral Resection of Bladder Tumor (TURBT): A procedure where a cystoscope is used to remove tumors from the bladder lining. This is often the first treatment for early-stage bladder cancer.
Transurethral Resection of Bladder Tumor (TURBT): A procedure where a cystoscope is used to remove tumors from the bladder lining. This is often the first treatment for early-stage bladder cancer.![]()

![]() Cystectomy: Surgical removal of all or part of the bladder.
Cystectomy: Surgical removal of all or part of the bladder.![]()

![]() Partial Cystectomy: Removal of only a portion of the bladder (used in select cases).
Partial Cystectomy: Removal of only a portion of the bladder (used in select cases).![]()

![]() Radical Cystectomy: Removal of the entire bladder, nearby lymph nodes, and sometimes nearby organs (e.g., prostate in men, uterus and ovaries in women). After a radical cystectomy, a new way to store and eliminate urine must be created (urinary diversion).
Radical Cystectomy: Removal of the entire bladder, nearby lymph nodes, and sometimes nearby organs (e.g., prostate in men, uterus and ovaries in women). After a radical cystectomy, a new way to store and eliminate urine must be created (urinary diversion).
![]() Intravesical Therapy: Medication is delivered directly into the bladder through a catheter. This is often used after TURBT for early-stage bladder cancer to prevent recurrence.
Intravesical Therapy: Medication is delivered directly into the bladder through a catheter. This is often used after TURBT for early-stage bladder cancer to prevent recurrence.![]()

![]() Immunotherapy (BCG): Bacillus Calmette-Guérin (BCG) is a weakened form of bacteria that stimulates the immune system to attack cancer cells.
Immunotherapy (BCG): Bacillus Calmette-Guérin (BCG) is a weakened form of bacteria that stimulates the immune system to attack cancer cells.![]()

![]() Chemotherapy: Chemotherapy drugs can be used directly into the bladder.
Chemotherapy: Chemotherapy drugs can be used directly into the bladder.
![]() Systemic Chemotherapy: Chemotherapy drugs are given intravenously (through a vein) to kill cancer cells throughout the body. This is typically used for more advanced bladder cancer.
Systemic Chemotherapy: Chemotherapy drugs are given intravenously (through a vein) to kill cancer cells throughout the body. This is typically used for more advanced bladder cancer.
![]() Radiation Therapy: High-energy rays are used to kill cancer cells. Radiation therapy can be used alone or in combination with other treatments.
Radiation Therapy: High-energy rays are used to kill cancer cells. Radiation therapy can be used alone or in combination with other treatments.
![]() Immunotherapy: Drugs that help the body's immune system fight cancer. These drugs may be used for advanced bladder cancer.
Immunotherapy: Drugs that help the body's immune system fight cancer. These drugs may be used for advanced bladder cancer.
![]() Targeted Therapy: Drugs that target specific abnormalities in cancer cells.
Targeted Therapy: Drugs that target specific abnormalities in cancer cells.
Follow-up Care:
After treatment, regular follow-up appointments and tests are important to monitor for recurrence.
Prevention:
![]() Don't smoke: This is the most important thing you can do to reduce your risk.
Don't smoke: This is the most important thing you can do to reduce your risk.
![]() Avoid exposure to certain chemicals: If you work with chemicals, follow safety precautions.
Avoid exposure to certain chemicals: If you work with chemicals, follow safety precautions.
![]() Drink plenty of water: This helps to flush out toxins from the bladder.
Drink plenty of water: This helps to flush out toxins from the bladder.
![]() Eat a healthy diet: A diet rich in fruits and vegetables may help to reduce your risk.
Eat a healthy diet: A diet rich in fruits and vegetables may help to reduce your risk.
![]() Talk to your doctor: If you have any risk factors or symptoms of bladder cancer, talk to your doctor.
Talk to your doctor: If you have any risk factors or symptoms of bladder cancer, talk to your doctor.
Important Considerations:
![]() Early detection is crucial for successful treatment.
Early detection is crucial for successful treatment.
![]() Treatment options are constantly evolving.
Treatment options are constantly evolving.
![]() A multidisciplinary team of doctors, including urologists, oncologists, and radiation oncologists, is often involved in the care of people with bladder cancer.
A multidisciplinary team of doctors, including urologists, oncologists, and radiation oncologists, is often involved in the care of people with bladder cancer.
![]() Quality of life is an important consideration when making treatment decisions, especially regarding urinary diversion after cystectomy.
Quality of life is an important consideration when making treatment decisions, especially regarding urinary diversion after cystectomy.
Disclaimer: This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.