Bladder outlet obstruction (Obstructive uropathy)
Published: 18 Jun 2025
ICD9: 599.60 ICD10: N13.9 ICD11: GC01.0
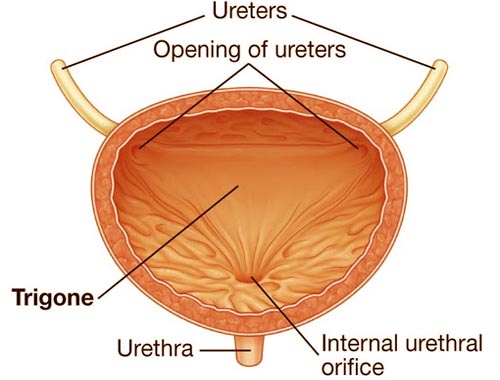
Bladder outlet obstruction (BOO), also known as obstructive uropathy, is a blockage at the base of the bladder that reduces or stops the flow of urine from the bladder into the urethra.
Think of it as a kink in the garden hose preventing water from flowing freely.
Here's a breakdown:
![]() Bladder Outlet: This is the point where the bladder connects to the urethra (the tube that carries urine out of the body).
Bladder Outlet: This is the point where the bladder connects to the urethra (the tube that carries urine out of the body).
![]() Obstruction: Something is blocking or narrowing this outlet, making it difficult for urine to pass.
Obstruction: Something is blocking or narrowing this outlet, making it difficult for urine to pass.
![]() Obstructive Uropathy: This is a more general term that refers to any blockage in the urinary tract, which includes BOO but can also include obstructions higher up, such as in the ureters (tubes connecting the kidneys to the bladder).
Obstructive Uropathy: This is a more general term that refers to any blockage in the urinary tract, which includes BOO but can also include obstructions higher up, such as in the ureters (tubes connecting the kidneys to the bladder).
What causes Bladder Outlet Obstruction?
There are several possible causes, and they can differ in men and women:
Common in Men:
![]() Benign Prostatic Hyperplasia (BPH): This is the most common cause. An enlarged prostate gland presses on the urethra, narrowing the opening.
Benign Prostatic Hyperplasia (BPH): This is the most common cause. An enlarged prostate gland presses on the urethra, narrowing the opening.
![]() Prostate Cancer: Less common than BPH, but prostate cancer can also obstruct the urethra.
Prostate Cancer: Less common than BPH, but prostate cancer can also obstruct the urethra.
![]() Urethral stricture: Scar tissue in the urethra can cause narrowing.
Urethral stricture: Scar tissue in the urethra can cause narrowing.
Common in Women:
![]() Pelvic organ prolapse: When organs in the pelvis (like the bladder or uterus) drop out of place, they can compress the urethra.
Pelvic organ prolapse: When organs in the pelvis (like the bladder or uterus) drop out of place, they can compress the urethra.
![]() Urethral stricture: Less common in women than men, but it can occur.
Urethral stricture: Less common in women than men, but it can occur.
![]() Bladder neck contracture: Scarring and tightening of the bladder neck (the area where the bladder connects to the urethra).
Bladder neck contracture: Scarring and tightening of the bladder neck (the area where the bladder connects to the urethra).
Less common causes (affecting both men and women):
![]() Bladder stones: A stone can block the outlet.
Bladder stones: A stone can block the outlet.
![]() Tumors: Tumors in the bladder or urethra can cause obstruction.
Tumors: Tumors in the bladder or urethra can cause obstruction.
![]() Nerve damage (neurogenic bladder): Nerve problems can interfere with bladder muscle function, leading to difficulty emptying and, potentially, obstruction.
Nerve damage (neurogenic bladder): Nerve problems can interfere with bladder muscle function, leading to difficulty emptying and, potentially, obstruction.
![]() Medications: Some medications can affect bladder function.
Medications: Some medications can affect bladder function.
Symptoms of Bladder Outlet Obstruction:
Symptoms can vary depending on the severity of the obstruction, but common ones include:
![]() Weak urine stream: The force of the urine is reduced.
Weak urine stream: The force of the urine is reduced.
![]() Straining to urinate: You have to push or bear down to start the flow.
Straining to urinate: You have to push or bear down to start the flow.
![]() Hesitancy: Difficulty starting the urine stream.
Hesitancy: Difficulty starting the urine stream.
![]() Intermittency: The urine stream stops and starts.
Intermittency: The urine stream stops and starts.
![]() Frequency: Needing to urinate often.
Frequency: Needing to urinate often.
![]() Urgency: A sudden, strong urge to urinate.
Urgency: A sudden, strong urge to urinate.
![]() Nocturia: Waking up frequently at night to urinate.
Nocturia: Waking up frequently at night to urinate.
![]() Feeling of incomplete bladder emptying: Feeling like you haven't completely emptied your bladder, even after urinating.
Feeling of incomplete bladder emptying: Feeling like you haven't completely emptied your bladder, even after urinating.
![]() Dribbling: Leaking urine after urination.
Dribbling: Leaking urine after urination.
![]() Urinary retention: Inability to urinate at all (this is a medical emergency).
Urinary retention: Inability to urinate at all (this is a medical emergency).
![]() Recurrent Urinary tract infections (UTIs).
Recurrent Urinary tract infections (UTIs).
![]() Overflow incontinence: Leaking urine because the bladder is too full.
Overflow incontinence: Leaking urine because the bladder is too full.
Diagnosis:
Diagnosing BOO typically involves:
![]() Medical history and physical exam: The doctor will ask about your symptoms and perform a physical examination.
Medical history and physical exam: The doctor will ask about your symptoms and perform a physical examination.
![]() Urinalysis: To check for infection or other abnormalities.
Urinalysis: To check for infection or other abnormalities.
![]() Post-void residual (PVR) measurement: This measures the amount of urine left in your bladder after urination. A high PVR suggests incomplete emptying.
Post-void residual (PVR) measurement: This measures the amount of urine left in your bladder after urination. A high PVR suggests incomplete emptying.
![]() Uroflowmetry: This measures the rate and volume of urine flow.
Uroflowmetry: This measures the rate and volume of urine flow.
![]() Cystoscopy: A thin, flexible tube with a camera is inserted into the urethra to visualize the bladder and urethra.
Cystoscopy: A thin, flexible tube with a camera is inserted into the urethra to visualize the bladder and urethra.
![]() Imaging studies: Ultrasound, CT scans, or MRI scans may be used to visualize the urinary tract and identify the cause of the obstruction.
Imaging studies: Ultrasound, CT scans, or MRI scans may be used to visualize the urinary tract and identify the cause of the obstruction.
Treatment:
Treatment depends on the cause and severity of the obstruction. Options may include:
![]() Medications:
Medications:![]()

![]() Alpha-blockers (for BPH): These relax the muscles in the prostate and bladder neck.
Alpha-blockers (for BPH): These relax the muscles in the prostate and bladder neck.![]()

![]() 5-alpha reductase inhibitors (for BPH): These shrink the prostate gland.
5-alpha reductase inhibitors (for BPH): These shrink the prostate gland.![]()

![]() Antibiotics (if infection is present).
Antibiotics (if infection is present).
![]() Catheterization: Inserting a catheter into the bladder to drain urine. This may be temporary or long-term, depending on the situation.
Catheterization: Inserting a catheter into the bladder to drain urine. This may be temporary or long-term, depending on the situation.
![]() Surgery:
Surgery:![]()

![]() Transurethral resection of the prostate (TURP): A common procedure for BPH that involves removing part of the prostate gland.
Transurethral resection of the prostate (TURP): A common procedure for BPH that involves removing part of the prostate gland.![]()

![]() Other surgical procedures to correct urethral strictures, remove bladder stones or tumors, or repair pelvic organ prolapse.
Other surgical procedures to correct urethral strictures, remove bladder stones or tumors, or repair pelvic organ prolapse.
![]() Lifestyle modifications: For mild cases, lifestyle changes such as timed voiding, double voiding, and fluid management might be helpful.
Lifestyle modifications: For mild cases, lifestyle changes such as timed voiding, double voiding, and fluid management might be helpful.
Complications:
If left untreated, BOO can lead to serious complications, including:
![]() Urinary retention
Urinary retention
![]() Urinary tract infections (UTIs)
Urinary tract infections (UTIs)
![]() Bladder damage: Chronic overdistension of the bladder can damage its muscles.
Bladder damage: Chronic overdistension of the bladder can damage its muscles.
![]() Kidney damage (hydronephrosis): Backflow of urine can damage the kidneys.
Kidney damage (hydronephrosis): Backflow of urine can damage the kidneys.
![]() Kidney failure
Kidney failure
In summary, Bladder outlet obstruction is a condition where something blocks the flow of urine from the bladder. It's important to see a doctor if you're experiencing symptoms of BOO so that the cause can be identified and treated to prevent complications.
Disclaimer: This information is for general knowledge only and should not be considered medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition.