Bone Marrow Disorders (Myelodysplasia, Myelodysplastic syndromes)
Published: 18 Jun 2025
ICD9: 238.75 ICD10: D46.9 ICD11: 2A3Z
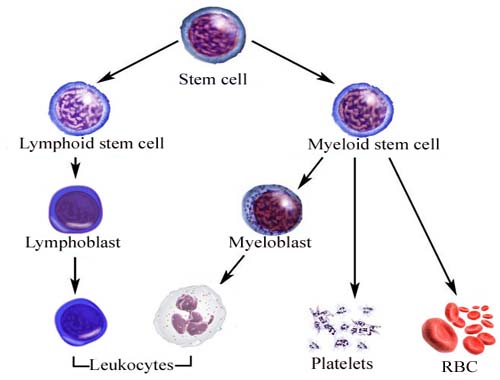
Bone marrow disorders, specifically myelodysplasia and myelodysplastic syndromes (MDS), represent a group of diseases where the bone marrow fails to produce enough healthy blood cells.
Instead, the bone marrow produces immature, abnormal cells (called blasts) that don't function properly. This leads to a deficiency in one or more types of blood cells: red blood cells (causing anemia), white blood cells (increasing susceptibility to infections), and platelets (leading to bleeding problems).
Here's a breakdown of key aspects:
![]() Myelodysplastic Syndromes (MDS): This is the umbrella term for a collection of related disorders. They are characterized by:
Myelodysplastic Syndromes (MDS): This is the umbrella term for a collection of related disorders. They are characterized by:![]()

![]() Ineffective hematopoiesis: The bone marrow is working, but the blood cells it produces are abnormal and often die before leaving the marrow, or they are quickly destroyed in the bloodstream.
Ineffective hematopoiesis: The bone marrow is working, but the blood cells it produces are abnormal and often die before leaving the marrow, or they are quickly destroyed in the bloodstream.![]()

![]() Cytopenias: Low blood cell counts (one or more of red blood cells, white blood cells, or platelets).
Cytopenias: Low blood cell counts (one or more of red blood cells, white blood cells, or platelets).![]()

![]() Dysplasia: Abnormal appearance and development of blood cells in the bone marrow. These cells look different under a microscope.
Dysplasia: Abnormal appearance and development of blood cells in the bone marrow. These cells look different under a microscope.![]()

![]() Risk of progression to acute myeloid leukemia (AML): MDS can transform into AML, a more aggressive form of blood cancer, in some cases.
Risk of progression to acute myeloid leukemia (AML): MDS can transform into AML, a more aggressive form of blood cancer, in some cases.
![]() Causes: The exact cause of MDS is often unknown (idiopathic). However, some known risk factors include:
Causes: The exact cause of MDS is often unknown (idiopathic). However, some known risk factors include:![]()

![]() Prior chemotherapy or radiation therapy: Treatment for other cancers can damage the bone marrow and increase the risk of MDS.
Prior chemotherapy or radiation therapy: Treatment for other cancers can damage the bone marrow and increase the risk of MDS.![]()

![]() Exposure to certain chemicals: Benzene and other industrial chemicals have been linked to MDS.
Exposure to certain chemicals: Benzene and other industrial chemicals have been linked to MDS.![]()

![]() Genetic factors: Some rare inherited conditions can predispose individuals to MDS. Some genetic mutations also develop spontaneously (de novo) in bone marrow cells.
Genetic factors: Some rare inherited conditions can predispose individuals to MDS. Some genetic mutations also develop spontaneously (de novo) in bone marrow cells.![]()

![]() Age: MDS is more common in older adults, typically over 60.
Age: MDS is more common in older adults, typically over 60.
![]() Symptoms: Symptoms vary depending on which blood cells are deficient. Common symptoms include:
Symptoms: Symptoms vary depending on which blood cells are deficient. Common symptoms include:![]()

![]() Fatigue: Due to anemia (low red blood cell count).
Fatigue: Due to anemia (low red blood cell count).![]()

![]() Shortness of breath: Also due to anemia.
Shortness of breath: Also due to anemia.![]()

![]() Frequent infections: Due to low white blood cell count (neutropenia).
Frequent infections: Due to low white blood cell count (neutropenia).![]()

![]() Easy bruising or bleeding: Due to low platelet count (thrombocytopenia).
Easy bruising or bleeding: Due to low platelet count (thrombocytopenia).![]()

![]() Pale skin: Due to anemia.
Pale skin: Due to anemia.![]()

![]() Petechiae: Small, pinpoint-sized red or purple spots on the skin, caused by bleeding under the skin.
Petechiae: Small, pinpoint-sized red or purple spots on the skin, caused by bleeding under the skin.
![]() Diagnosis: Diagnosis typically involves:
Diagnosis: Diagnosis typically involves:![]()

![]() Complete blood count (CBC): To assess the levels of red blood cells, white blood cells, and platelets.
Complete blood count (CBC): To assess the levels of red blood cells, white blood cells, and platelets.![]()

![]() Peripheral blood smear: To examine the appearance of blood cells under a microscope.
Peripheral blood smear: To examine the appearance of blood cells under a microscope.![]()

![]() Bone marrow aspiration and biopsy: Essential for confirming the diagnosis and evaluating the proportion of blast cells and the degree of dysplasia. The bone marrow sample is also used for cytogenetic and molecular testing.
Bone marrow aspiration and biopsy: Essential for confirming the diagnosis and evaluating the proportion of blast cells and the degree of dysplasia. The bone marrow sample is also used for cytogenetic and molecular testing.![]()

![]() Cytogenetic analysis: To look for chromosomal abnormalities in the bone marrow cells.
Cytogenetic analysis: To look for chromosomal abnormalities in the bone marrow cells.![]()

![]() Molecular testing: To identify specific gene mutations associated with MDS.
Molecular testing: To identify specific gene mutations associated with MDS.
![]() Treatment: Treatment options depend on the severity of the MDS, the risk of progression to AML, and the patient's overall health. Options include:
Treatment: Treatment options depend on the severity of the MDS, the risk of progression to AML, and the patient's overall health. Options include:![]()

![]() Supportive care: Blood transfusions to manage anemia, antibiotics to treat infections, and platelet transfusions to control bleeding.
Supportive care: Blood transfusions to manage anemia, antibiotics to treat infections, and platelet transfusions to control bleeding.![]()

![]() Growth factors: Medications that stimulate the bone marrow to produce more blood cells (e.g., erythropoietin for anemia, G-CSF for neutropenia).
Growth factors: Medications that stimulate the bone marrow to produce more blood cells (e.g., erythropoietin for anemia, G-CSF for neutropenia).![]()

![]() Hypomethylating agents (HMAs): Drugs like azacitidine and decitabine that can help to improve blood cell production and reduce the risk of progression to AML.
Hypomethylating agents (HMAs): Drugs like azacitidine and decitabine that can help to improve blood cell production and reduce the risk of progression to AML.![]()

![]() Lenalidomide: A drug that can be effective in patients with a specific chromosomal abnormality (deletion 5q).
Lenalidomide: A drug that can be effective in patients with a specific chromosomal abnormality (deletion 5q).![]()

![]() Stem cell transplantation (bone marrow transplant): The only potentially curative treatment option. It involves replacing the patient's abnormal bone marrow with healthy stem cells from a donor. This is often considered for younger, healthier patients with higher-risk MDS.
Stem cell transplantation (bone marrow transplant): The only potentially curative treatment option. It involves replacing the patient's abnormal bone marrow with healthy stem cells from a donor. This is often considered for younger, healthier patients with higher-risk MDS.![]()

![]() Clinical trials: Participation in clinical trials may offer access to new and experimental therapies.
Clinical trials: Participation in clinical trials may offer access to new and experimental therapies.
![]() Prognosis: The prognosis for MDS varies widely. Factors that affect prognosis include the subtype of MDS, the degree of dysplasia, the presence of chromosomal abnormalities, the number of blast cells in the bone marrow, and the patient's age and overall health. Risk scoring systems, such as the IPSS-R (Revised International Prognostic Scoring System), are used to estimate the prognosis and guide treatment decisions.
Prognosis: The prognosis for MDS varies widely. Factors that affect prognosis include the subtype of MDS, the degree of dysplasia, the presence of chromosomal abnormalities, the number of blast cells in the bone marrow, and the patient's age and overall health. Risk scoring systems, such as the IPSS-R (Revised International Prognostic Scoring System), are used to estimate the prognosis and guide treatment decisions.
In summary: Myelodysplastic syndromes are a group of bone marrow disorders characterized by ineffective blood cell production, resulting in low blood cell counts and an increased risk of developing acute myeloid leukemia. Diagnosis involves blood and bone marrow tests, and treatment options range from supportive care to stem cell transplantation.