Cardiomyopathy
Published: 18 Jun 2025
ICD9: 425.18 ICD10: I42.2 ICD11: BC43
Cardiomyopathy is a general term for diseases of the heart muscle.
These diseases can make it harder for the heart to pump blood to the rest of the body. Cardiomyopathy can lead to heart failure.
Here's a more detailed breakdown:
What it is:
![]() "Cardio" refers to the heart.
"Cardio" refers to the heart.
![]() "Myo" refers to muscle.
"Myo" refers to muscle.
![]() "Pathy" refers to disease.
"Pathy" refers to disease.
So, cardiomyopathy literally means "heart muscle disease." It affects the structure and function of the heart muscle, making it difficult for the heart to pump blood effectively.
How it affects the heart:
Cardiomyopathy can affect the heart in several ways:
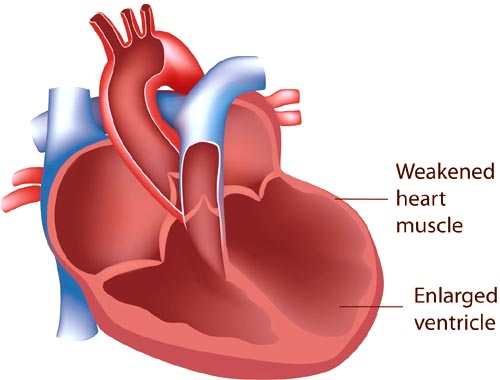
![]() Enlarging the heart (Dilated Cardiomyopathy): The heart chambers, particularly the left ventricle, become enlarged and weakened. This is the most common type.
Enlarging the heart (Dilated Cardiomyopathy): The heart chambers, particularly the left ventricle, become enlarged and weakened. This is the most common type.
![]() Thickening the heart muscle (Hypertrophic Cardiomyopathy): The heart muscle becomes abnormally thick, making it harder for the heart to pump blood. This thickening can obstruct blood flow out of the heart.
Thickening the heart muscle (Hypertrophic Cardiomyopathy): The heart muscle becomes abnormally thick, making it harder for the heart to pump blood. This thickening can obstruct blood flow out of the heart.
![]() Making the heart muscle rigid (Restrictive Cardiomyopathy): The heart muscle becomes stiff and less flexible, restricting the heart's ability to fill with blood between heartbeats.
Making the heart muscle rigid (Restrictive Cardiomyopathy): The heart muscle becomes stiff and less flexible, restricting the heart's ability to fill with blood between heartbeats.
![]() Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): The heart muscle is replaced by fat and fibrous tissue, primarily in the right ventricle. This disrupts the heart's electrical signals and can lead to arrhythmias.
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): The heart muscle is replaced by fat and fibrous tissue, primarily in the right ventricle. This disrupts the heart's electrical signals and can lead to arrhythmias.
![]() Unclassified Cardiomyopathies: Some cardiomyopathies don't fit neatly into the above categories.
Unclassified Cardiomyopathies: Some cardiomyopathies don't fit neatly into the above categories.
Causes:
The causes of cardiomyopathy vary depending on the type:
![]() Dilated Cardiomyopathy:
Dilated Cardiomyopathy:![]()

![]() Genetics (family history)
Genetics (family history)![]()

![]() Coronary artery disease
Coronary artery disease![]()

![]() High blood pressure
High blood pressure![]()

![]() Heart valve problems
Heart valve problems![]()

![]() Viral infections
Viral infections![]()

![]() Alcohol abuse
Alcohol abuse![]()

![]() Drug abuse (e.g., cocaine)
Drug abuse (e.g., cocaine)![]()

![]() Certain medications
Certain medications![]()

![]() Pregnancy (peripartum cardiomyopathy)
Pregnancy (peripartum cardiomyopathy)
![]() Hypertrophic Cardiomyopathy:
Hypertrophic Cardiomyopathy:![]()

![]() Genetics (family history) - often the primary cause
Genetics (family history) - often the primary cause
![]() Restrictive Cardiomyopathy:
Restrictive Cardiomyopathy:![]()

![]() Amyloidosis (abnormal protein deposits)
Amyloidosis (abnormal protein deposits)![]()

![]() Sarcoidosis (inflammatory disease)
Sarcoidosis (inflammatory disease)![]()

![]() Hemochromatosis (iron overload)
Hemochromatosis (iron overload)![]()

![]() Scar tissue formation after heart surgery or radiation
Scar tissue formation after heart surgery or radiation![]()

![]() In some cases, the cause is unknown (idiopathic)
In some cases, the cause is unknown (idiopathic)
![]() Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC):
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC):![]()

![]() Genetics (family history)
Genetics (family history)![]()

![]() May be triggered or worsened by intense, prolonged exercise.
May be triggered or worsened by intense, prolonged exercise.
Symptoms:
Many people with cardiomyopathy have no symptoms, especially in the early stages. When symptoms do occur, they can include:
![]() Shortness of breath, especially with exertion or lying down
Shortness of breath, especially with exertion or lying down
![]() Fatigue
Fatigue
![]() Swelling in the ankles, feet, legs, or abdomen
Swelling in the ankles, feet, legs, or abdomen
![]() Dizziness, lightheadedness, or fainting
Dizziness, lightheadedness, or fainting
![]() Chest pain or pressure
Chest pain or pressure
![]() Heart palpitations (a feeling of rapid, fluttering, or pounding heartbeat)
Heart palpitations (a feeling of rapid, fluttering, or pounding heartbeat)
![]() Cough
Cough
![]() Irregular heartbeat (arrhythmia)
Irregular heartbeat (arrhythmia)
Diagnosis:
Diagnosis typically involves:
![]() Physical exam: Listening to the heart and lungs.
Physical exam: Listening to the heart and lungs.
![]() Echocardiogram: An ultrasound of the heart to assess its size, shape, and function.
Echocardiogram: An ultrasound of the heart to assess its size, shape, and function.
![]() Electrocardiogram (ECG or EKG): Measures the electrical activity of the heart.
Electrocardiogram (ECG or EKG): Measures the electrical activity of the heart.
![]() Chest X-ray: Shows the size and shape of the heart and lungs.
Chest X-ray: Shows the size and shape of the heart and lungs.
![]() Cardiac MRI: Provides detailed images of the heart.
Cardiac MRI: Provides detailed images of the heart.
![]() Blood tests: To rule out other conditions and assess heart function.
Blood tests: To rule out other conditions and assess heart function.
![]() Cardiac catheterization: A procedure where a thin tube is inserted into a blood vessel and guided to the heart. This can measure pressures in the heart and take samples.
Cardiac catheterization: A procedure where a thin tube is inserted into a blood vessel and guided to the heart. This can measure pressures in the heart and take samples.
![]() Genetic testing: To identify gene mutations that can cause cardiomyopathy.
Genetic testing: To identify gene mutations that can cause cardiomyopathy.
![]() Endomyocardial biopsy: A small sample of heart tissue is taken for examination under a microscope (less commonly performed).
Endomyocardial biopsy: A small sample of heart tissue is taken for examination under a microscope (less commonly performed).
Treatment:
Treatment depends on the type and severity of the cardiomyopathy and the symptoms. Goals of treatment include:
![]() Managing symptoms
Managing symptoms
![]() Preventing complications (like heart failure, blood clots, arrhythmias, and sudden cardiac death)
Preventing complications (like heart failure, blood clots, arrhythmias, and sudden cardiac death)
![]() Slowing the progression of the disease
Slowing the progression of the disease
Treatment options may include:
![]() Medications:
Medications:![]()

![]() ACE inhibitors or ARBs (to lower blood pressure and improve heart function)
ACE inhibitors or ARBs (to lower blood pressure and improve heart function)![]()

![]() Beta-blockers (to slow the heart rate and lower blood pressure)
Beta-blockers (to slow the heart rate and lower blood pressure)![]()

![]() Diuretics (to reduce fluid buildup)
Diuretics (to reduce fluid buildup)![]()

![]() Digoxin (to strengthen heart contractions)
Digoxin (to strengthen heart contractions)![]()

![]() Antiarrhythmic medications (to control irregular heartbeats)
Antiarrhythmic medications (to control irregular heartbeats)![]()

![]() Anticoagulants (to prevent blood clots)
Anticoagulants (to prevent blood clots)
![]() Lifestyle changes:
Lifestyle changes:![]()

![]() Low-sodium diet
Low-sodium diet![]()

![]() Fluid restriction
Fluid restriction![]()

![]() Regular exercise (as advised by a doctor)
Regular exercise (as advised by a doctor)![]()

![]() Avoiding alcohol and tobacco
Avoiding alcohol and tobacco![]()

![]() Weight management
Weight management![]()

![]() Stress management
Stress management
![]() Implantable devices:
Implantable devices:![]()

![]() Pacemaker (to regulate heart rhythm)
Pacemaker (to regulate heart rhythm)![]()

![]() Implantable cardioverter-defibrillator (ICD) (to deliver an electric shock if a life-threatening arrhythmia occurs)
Implantable cardioverter-defibrillator (ICD) (to deliver an electric shock if a life-threatening arrhythmia occurs)![]()

![]() Cardiac resynchronization therapy (CRT) (a special type of pacemaker to coordinate the contractions of the ventricles)
Cardiac resynchronization therapy (CRT) (a special type of pacemaker to coordinate the contractions of the ventricles)
![]() Surgery or other procedures:
Surgery or other procedures:![]()

![]() Septal myectomy (for hypertrophic cardiomyopathy, to remove thickened heart muscle)
Septal myectomy (for hypertrophic cardiomyopathy, to remove thickened heart muscle)![]()

![]() Alcohol septal ablation (for hypertrophic cardiomyopathy, to destroy thickened heart muscle with alcohol)
Alcohol septal ablation (for hypertrophic cardiomyopathy, to destroy thickened heart muscle with alcohol)![]()

![]() Heart transplant (in severe cases of heart failure)
Heart transplant (in severe cases of heart failure)![]()

![]() Ventricular assist device (VAD) (a mechanical pump to help the heart circulate blood)
Ventricular assist device (VAD) (a mechanical pump to help the heart circulate blood)
![]() For ARVC: Catheter ablation to destroy abnormal electrical pathways in the heart.
For ARVC: Catheter ablation to destroy abnormal electrical pathways in the heart.
Prognosis:
The prognosis for cardiomyopathy varies depending on the type, severity, and response to treatment. Some people can live long and relatively normal lives with medication and lifestyle changes. Others may develop more serious complications, such as heart failure or sudden cardiac death. Regular follow-up with a cardiologist is essential.
In summary, cardiomyopathy is a serious disease that affects the heart muscle. Early diagnosis and treatment are crucial to manage symptoms, prevent complications, and improve the quality of life for those affected.
![]() Disclaimer: This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.*
Disclaimer: This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.*