Cirrhosis
Published: 18 Jun 2025
ICD9: 571.5 ICD10: K74.60 ICD11: DB93.1
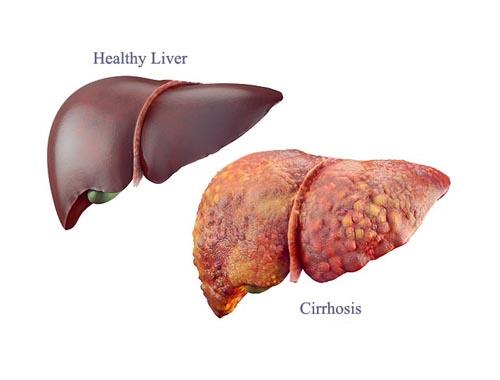
Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases and conditions, such as hepatitis and chronic alcohol abuse.
Here's a breakdown:
![]() What it is: Cirrhosis is a progressive disease where healthy liver tissue is replaced with scar tissue. This scar tissue blocks the flow of blood through the liver and slows down the liver's ability to process nutrients, hormones, drugs, and toxins.
What it is: Cirrhosis is a progressive disease where healthy liver tissue is replaced with scar tissue. This scar tissue blocks the flow of blood through the liver and slows down the liver's ability to process nutrients, hormones, drugs, and toxins.
![]() Cause: It's the result of long-term damage to the liver. Common causes include:
Cause: It's the result of long-term damage to the liver. Common causes include:![]()

![]() Chronic alcohol abuse: Excessive alcohol consumption over many years.
Chronic alcohol abuse: Excessive alcohol consumption over many years.![]()

![]() Chronic viral hepatitis: Hepatitis B, C, and D infections.
Chronic viral hepatitis: Hepatitis B, C, and D infections.![]()

![]() Nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): Fat buildup in the liver, not related to alcohol.
Nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): Fat buildup in the liver, not related to alcohol.![]()

![]() Autoimmune liver diseases: Autoimmune hepatitis, primary biliary cholangitis, and primary sclerosing cholangitis.
Autoimmune liver diseases: Autoimmune hepatitis, primary biliary cholangitis, and primary sclerosing cholangitis.![]()

![]() Genetic diseases: Hemochromatosis, Wilson's disease, alpha-1 antitrypsin deficiency.
Genetic diseases: Hemochromatosis, Wilson's disease, alpha-1 antitrypsin deficiency.![]()

![]() Certain drugs, toxins, and infections
Certain drugs, toxins, and infections![]()

![]() Blocked bile ducts
Blocked bile ducts![]()

![]() Repeated bouts of heart failure with liver congestion
Repeated bouts of heart failure with liver congestion
![]() Symptoms: In early stages, there may be few or no symptoms. As cirrhosis progresses, symptoms can include:
Symptoms: In early stages, there may be few or no symptoms. As cirrhosis progresses, symptoms can include:![]()

![]() Fatigue
Fatigue![]()

![]() Weakness
Weakness![]()

![]() Loss of appetite
Loss of appetite![]()

![]() Nausea
Nausea![]()

![]() Weight loss
Weight loss![]()

![]() Jaundice (yellowing of the skin and eyes)
Jaundice (yellowing of the skin and eyes)![]()

![]() Itching
Itching![]()

![]() Swelling in the legs, feet, or ankles (edema)
Swelling in the legs, feet, or ankles (edema)![]()

![]() Fluid buildup in the abdomen (ascites)
Fluid buildup in the abdomen (ascites)![]()

![]() Easy bruising or bleeding
Easy bruising or bleeding![]()

![]() Spider-like blood vessels on the skin
Spider-like blood vessels on the skin![]()

![]() Confusion, drowsiness, or slurred speech (hepatic encephalopathy)
Confusion, drowsiness, or slurred speech (hepatic encephalopathy)
![]() Complications: Cirrhosis can lead to serious complications, including:
Complications: Cirrhosis can lead to serious complications, including:![]()

![]() Portal hypertension: Increased pressure in the portal vein (the vein that carries blood from the digestive organs to the liver).
Portal hypertension: Increased pressure in the portal vein (the vein that carries blood from the digestive organs to the liver).![]()

![]() Varices: Enlarged veins in the esophagus or stomach that can bleed.
Varices: Enlarged veins in the esophagus or stomach that can bleed.![]()

![]() Ascites: Fluid buildup in the abdomen.
Ascites: Fluid buildup in the abdomen.![]()

![]() Hepatic encephalopathy: Brain damage due to the liver's inability to remove toxins from the blood.
Hepatic encephalopathy: Brain damage due to the liver's inability to remove toxins from the blood.![]()

![]() Splenomegaly: Enlargement of the spleen.
Splenomegaly: Enlargement of the spleen.![]()

![]() Kidney failure (hepatorenal syndrome)
Kidney failure (hepatorenal syndrome)![]()

![]() Liver cancer (hepatocellular carcinoma)
Liver cancer (hepatocellular carcinoma)![]()

![]() Infections
Infections![]()

![]() Malnutrition
Malnutrition![]()

![]() Bone disease
Bone disease
![]() Diagnosis: Diagnosis often involves:
Diagnosis: Diagnosis often involves:![]()

![]() Physical exam: A doctor will look for signs of liver disease.
Physical exam: A doctor will look for signs of liver disease.![]()

![]() Blood tests: To assess liver function.
Blood tests: To assess liver function.![]()

![]() Imaging tests: Ultrasound, CT scan, or MRI to visualize the liver.
Imaging tests: Ultrasound, CT scan, or MRI to visualize the liver.![]()

![]() Liver biopsy: A small sample of liver tissue is taken for examination.
Liver biopsy: A small sample of liver tissue is taken for examination.
![]() Treatment: Cirrhosis treatment focuses on:
Treatment: Cirrhosis treatment focuses on:![]()

![]() Slowing the progression of the disease: Addressing the underlying cause (e.g., treating hepatitis, abstaining from alcohol).
Slowing the progression of the disease: Addressing the underlying cause (e.g., treating hepatitis, abstaining from alcohol).![]()

![]() Managing symptoms and complications: Medications, lifestyle changes, and procedures may be needed.
Managing symptoms and complications: Medications, lifestyle changes, and procedures may be needed.![]()

![]() Liver transplant: In severe cases, a liver transplant may be necessary.
Liver transplant: In severe cases, a liver transplant may be necessary.
![]() Prevention: Preventing cirrhosis involves reducing risk factors:
Prevention: Preventing cirrhosis involves reducing risk factors:![]()

![]() Limit alcohol consumption: Or abstain from alcohol completely.
Limit alcohol consumption: Or abstain from alcohol completely.![]()

![]() Get vaccinated against hepatitis B.
Get vaccinated against hepatitis B.![]()

![]() Practice safe sex to prevent hepatitis C.
Practice safe sex to prevent hepatitis C.![]()

![]() Maintain a healthy weight to prevent NAFLD.
Maintain a healthy weight to prevent NAFLD.![]()

![]() Manage underlying medical conditions such as diabetes.
Manage underlying medical conditions such as diabetes.
It's important to consult with a doctor for any concerns about liver health or potential symptoms of cirrhosis. Early diagnosis and treatment can help slow the progression of the disease and improve outcomes.