Congestive Heart Failure
Published: 18 Jun 2025
ICD9: 428.0 ICD10: I50.9 ICD11: BD10
Congestive Heart Failure (CHF), often simply called Heart Failure, is a chronic, progressive condition in which the heart is unable to pump enough blood to meet the body's needs for blood and oxygen.
It doesn't mean the heart has stopped working entirely; it means the heart isn't pumping as strongly or efficiently as it should.
Here's a breakdown of the key aspects:
![]() The Problem: The heart can't pump enough blood. This can happen for a few reasons:
The Problem: The heart can't pump enough blood. This can happen for a few reasons:![]()

![]() The heart muscle is weak (Systolic Heart Failure or Heart Failure with reduced ejection fraction - HFrEF): The heart can't squeeze hard enough to push blood out effectively. Ejection fraction (the percentage of blood the heart pumps out with each beat) is low.
The heart muscle is weak (Systolic Heart Failure or Heart Failure with reduced ejection fraction - HFrEF): The heart can't squeeze hard enough to push blood out effectively. Ejection fraction (the percentage of blood the heart pumps out with each beat) is low.![]()

![]() The heart muscle is stiff (Diastolic Heart Failure or Heart Failure with preserved ejection fraction - HFpEF): The heart can't relax and fill properly with blood. Ejection fraction may be normal or near normal.
The heart muscle is stiff (Diastolic Heart Failure or Heart Failure with preserved ejection fraction - HFpEF): The heart can't relax and fill properly with blood. Ejection fraction may be normal or near normal.
![]() The Result: Because the heart isn't pumping effectively, blood and fluid back up into the:
The Result: Because the heart isn't pumping effectively, blood and fluid back up into the:![]()

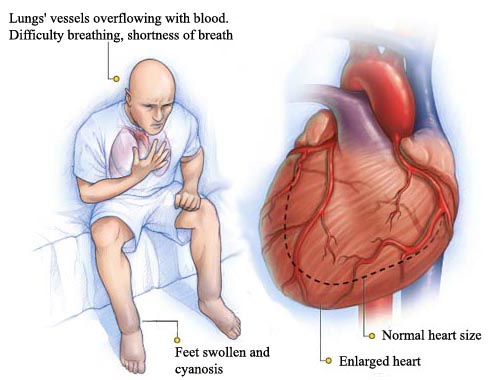
![]() Lungs: This causes shortness of breath (dyspnea), especially with exertion or when lying down, and can lead to coughing or wheezing.
Lungs: This causes shortness of breath (dyspnea), especially with exertion or when lying down, and can lead to coughing or wheezing.![]()

![]() Rest of the Body: This causes swelling (edema) in the legs, ankles, feet, abdomen (ascites), and veins in the neck. It can also lead to weight gain.
Rest of the Body: This causes swelling (edema) in the legs, ankles, feet, abdomen (ascites), and veins in the neck. It can also lead to weight gain.
![]() "Congestive" Part: The "congestive" part of the name comes from this buildup of fluid (congestion) in the lungs and other parts of the body.
"Congestive" Part: The "congestive" part of the name comes from this buildup of fluid (congestion) in the lungs and other parts of the body.
Causes of Heart Failure:
Many conditions can damage or weaken the heart, leading to heart failure. Common causes include:
![]() Coronary Artery Disease (CAD): Narrowed arteries reduce blood flow to the heart muscle. Heart attack (myocardial infarction) is a major cause.
Coronary Artery Disease (CAD): Narrowed arteries reduce blood flow to the heart muscle. Heart attack (myocardial infarction) is a major cause.
![]() High Blood Pressure (Hypertension): Forces the heart to work harder over time, leading to thickening of the heart muscle (hypertrophy).
High Blood Pressure (Hypertension): Forces the heart to work harder over time, leading to thickening of the heart muscle (hypertrophy).
![]() Valvular Heart Disease: Problems with the heart valves that control blood flow can strain the heart.
Valvular Heart Disease: Problems with the heart valves that control blood flow can strain the heart.
![]() Cardiomyopathy: Disease of the heart muscle itself, which can be caused by infections, alcohol abuse, drug abuse, genetic factors, or other conditions.
Cardiomyopathy: Disease of the heart muscle itself, which can be caused by infections, alcohol abuse, drug abuse, genetic factors, or other conditions.
![]() Congenital Heart Defects: Heart defects present at birth.
Congenital Heart Defects: Heart defects present at birth.
![]() Arrhythmias (Irregular Heartbeats): Can weaken the heart over time.
Arrhythmias (Irregular Heartbeats): Can weaken the heart over time.
![]() Diabetes: Increases the risk of heart disease and heart failure.
Diabetes: Increases the risk of heart disease and heart failure.
![]() Obesity: Puts extra strain on the heart.
Obesity: Puts extra strain on the heart.
![]() Severe Anemia: Low red blood cell count forces the heart to pump harder to deliver oxygen.
Severe Anemia: Low red blood cell count forces the heart to pump harder to deliver oxygen.
![]() Hyperthyroidism/Hypothyroidism: Thyroid problems can affect heart function.
Hyperthyroidism/Hypothyroidism: Thyroid problems can affect heart function.
Symptoms of Heart Failure:
Symptoms can vary depending on the severity of the heart failure and which side of the heart is primarily affected. Common symptoms include:
![]() Shortness of Breath (Dyspnea): Especially with exertion or when lying down (orthopnea). May also experience paroxysmal nocturnal dyspnea (sudden shortness of breath at night).
Shortness of Breath (Dyspnea): Especially with exertion or when lying down (orthopnea). May also experience paroxysmal nocturnal dyspnea (sudden shortness of breath at night).
![]() Fatigue and Weakness:
Fatigue and Weakness:
![]() Swelling (Edema): In the legs, ankles, feet, abdomen.
Swelling (Edema): In the legs, ankles, feet, abdomen.
![]() Rapid or Irregular Heartbeat: Palpitations.
Rapid or Irregular Heartbeat: Palpitations.
![]() Persistent Cough or Wheezing:
Persistent Cough or Wheezing:
![]() Weight Gain: Due to fluid retention.
Weight Gain: Due to fluid retention.
![]() Lack of Appetite or Nausea:
Lack of Appetite or Nausea:
![]() Increased Need to Urinate at Night:
Increased Need to Urinate at Night:
![]() Difficulty Concentrating or Decreased Alertness:
Difficulty Concentrating or Decreased Alertness:
Diagnosis:
Diagnosis typically involves a physical exam, medical history, and various tests, including:
![]() Echocardiogram: Ultrasound of the heart to assess its structure and function, including ejection fraction.
Echocardiogram: Ultrasound of the heart to assess its structure and function, including ejection fraction.
![]() Electrocardiogram (ECG or EKG): Measures electrical activity of the heart.
Electrocardiogram (ECG or EKG): Measures electrical activity of the heart.
![]() Chest X-ray: To look for fluid in the lungs or an enlarged heart.
Chest X-ray: To look for fluid in the lungs or an enlarged heart.
![]() Blood Tests: To check kidney function, electrolytes, and levels of certain hormones (e.g., BNP or NT-proBNP, which are elevated in heart failure).
Blood Tests: To check kidney function, electrolytes, and levels of certain hormones (e.g., BNP or NT-proBNP, which are elevated in heart failure).
![]() Stress Test: To assess how the heart functions during exercise.
Stress Test: To assess how the heart functions during exercise.
![]() Cardiac Catheterization: To check for blockages in the coronary arteries.
Cardiac Catheterization: To check for blockages in the coronary arteries.
Treatment:
Heart failure is a chronic condition that usually requires lifelong management. Treatment focuses on:
![]() Managing Symptoms: Relieving shortness of breath, swelling, and fatigue.
Managing Symptoms: Relieving shortness of breath, swelling, and fatigue.
![]() Treating Underlying Causes: Addressing conditions like high blood pressure, coronary artery disease, or valvular heart disease.
Treating Underlying Causes: Addressing conditions like high blood pressure, coronary artery disease, or valvular heart disease.
![]() Improving Heart Function: Slowing the progression of the disease and preventing further damage to the heart.
Improving Heart Function: Slowing the progression of the disease and preventing further damage to the heart.
![]() Reducing Hospitalizations:
Reducing Hospitalizations:
Treatment options include:
![]() Lifestyle Changes:
Lifestyle Changes:![]()

![]() Diet: Low-sodium diet, fluid restriction (if needed), healthy weight.
Diet: Low-sodium diet, fluid restriction (if needed), healthy weight.![]()

![]() Exercise: Regular physical activity, as tolerated. Cardiac rehabilitation programs can be very helpful.
Exercise: Regular physical activity, as tolerated. Cardiac rehabilitation programs can be very helpful.![]()

![]() Smoking Cessation:
Smoking Cessation:![]()

![]() Limiting Alcohol:
Limiting Alcohol:![]()

![]() Stress Management:
Stress Management:
![]() Medications: Several types of medications are used to treat heart failure, including:
Medications: Several types of medications are used to treat heart failure, including:![]()

![]() ACE inhibitors or ARBs or ARNIs: Help relax blood vessels and lower blood pressure.
ACE inhibitors or ARBs or ARNIs: Help relax blood vessels and lower blood pressure.![]()

![]() Beta-blockers: Slow heart rate and lower blood pressure.
Beta-blockers: Slow heart rate and lower blood pressure.![]()

![]() Diuretics (Water Pills): Help the body get rid of excess fluid.
Diuretics (Water Pills): Help the body get rid of excess fluid.![]()

![]() Aldosterone Antagonists: Also help the body get rid of excess fluid and can protect the heart.
Aldosterone Antagonists: Also help the body get rid of excess fluid and can protect the heart.![]()

![]() SGLT2 inhibitors: Originally developed for diabetes, these medications have been shown to improve outcomes in heart failure.
SGLT2 inhibitors: Originally developed for diabetes, these medications have been shown to improve outcomes in heart failure.![]()

![]() Digoxin: Helps the heart beat stronger.
Digoxin: Helps the heart beat stronger.![]()

![]() Ivabradine: Slows the heart rate.
Ivabradine: Slows the heart rate.
![]() Devices:
Devices:![]()

![]() Pacemaker: To regulate heart rhythm.
Pacemaker: To regulate heart rhythm.![]()

![]() Implantable Cardioverter-Defibrillator (ICD): To prevent sudden cardiac death.
Implantable Cardioverter-Defibrillator (ICD): To prevent sudden cardiac death.![]()

![]() Cardiac Resynchronization Therapy (CRT): A special type of pacemaker that helps coordinate the contractions of the heart chambers.
Cardiac Resynchronization Therapy (CRT): A special type of pacemaker that helps coordinate the contractions of the heart chambers.
![]() Surgery:
Surgery:![]()

![]() Coronary Artery Bypass Grafting (CABG): To bypass blocked coronary arteries.
Coronary Artery Bypass Grafting (CABG): To bypass blocked coronary arteries.![]()

![]() Valve Repair or Replacement:
Valve Repair or Replacement:![]()

![]() Heart Transplant: For severe heart failure that is not responding to other treatments.
Heart Transplant: For severe heart failure that is not responding to other treatments.![]()

![]() Ventricular Assist Device (VAD): A mechanical pump that helps the heart pump blood. Used as a bridge to transplant or as destination therapy.
Ventricular Assist Device (VAD): A mechanical pump that helps the heart pump blood. Used as a bridge to transplant or as destination therapy.
Prognosis:
Heart failure is a serious condition, and the prognosis (outlook) can vary depending on the severity of the disease, the underlying causes, and how well the patient adheres to treatment. With appropriate management, many people with heart failure can live long and productive lives. However, it's crucial to follow medical advice, take medications as prescribed, and adopt a healthy lifestyle.
Important Note: This information is for general knowledge and educational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment. Self-treating can be dangerous.