Crohn's Disease (Inflammatory Bowel Disease, IBD)
Published: 18 Jun 2025
ICD9: 555.9 ICD10: K50.90 ICD11: DD70
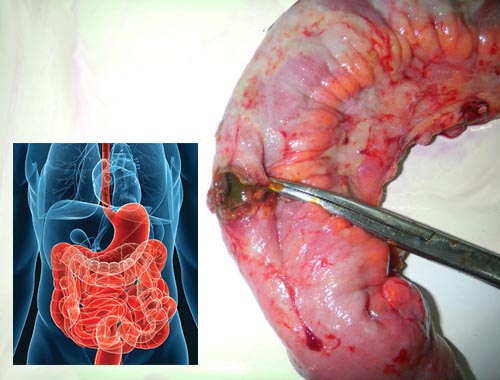
Crohn's Disease is a chronic inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal (GI) tract, from the mouth to the anus.
However, it most commonly affects the small intestine and the beginning of the colon.
Here's a breakdown of key aspects:
Key Characteristics:
![]() Inflammation: The hallmark of Crohn's is inflammation. This inflammation is chronic (long-lasting) and can lead to a variety of symptoms.
Inflammation: The hallmark of Crohn's is inflammation. This inflammation is chronic (long-lasting) and can lead to a variety of symptoms.
![]() Location: Unlike ulcerative colitis (another IBD), which is typically limited to the colon, Crohn's can occur anywhere in the digestive tract.
Location: Unlike ulcerative colitis (another IBD), which is typically limited to the colon, Crohn's can occur anywhere in the digestive tract.
![]() Transmural: Crohn's inflammation isn't just on the surface of the GI tract lining; it can extend through the entire thickness of the bowel wall (transmural).
Transmural: Crohn's inflammation isn't just on the surface of the GI tract lining; it can extend through the entire thickness of the bowel wall (transmural).
![]() Skip Lesions: The inflammation often occurs in patches, with areas of healthy tissue in between, referred to as "skip lesions." Imagine sections of the intestine being inflamed, then normal, then inflamed again.
Skip Lesions: The inflammation often occurs in patches, with areas of healthy tissue in between, referred to as "skip lesions." Imagine sections of the intestine being inflamed, then normal, then inflamed again.
![]() Granulomas: Microscopic examination of affected tissue often reveals granulomas, which are clusters of immune cells. While not always present, they are strongly associated with Crohn's.
Granulomas: Microscopic examination of affected tissue often reveals granulomas, which are clusters of immune cells. While not always present, they are strongly associated with Crohn's.
Symptoms:
Symptoms can vary widely depending on the location and severity of the inflammation, but common symptoms include:
![]() Abdominal pain and cramping: Often described as a colicky or crampy pain.
Abdominal pain and cramping: Often described as a colicky or crampy pain.
![]() Diarrhea: Can be frequent and sometimes bloody.
Diarrhea: Can be frequent and sometimes bloody.
![]() Rectal bleeding:
Rectal bleeding:
![]() Weight loss: Due to poor absorption of nutrients.
Weight loss: Due to poor absorption of nutrients.
![]() Fatigue:
Fatigue:
![]() Fever:
Fever:
![]() Loss of appetite:
Loss of appetite:
![]() Nausea and vomiting:
Nausea and vomiting:
![]() Mouth sores: Aphthous ulcers (canker sores) can occur.
Mouth sores: Aphthous ulcers (canker sores) can occur.
![]() Perianal disease: Anal fissures, fistulas, and abscesses are common in Crohn's disease.
Perianal disease: Anal fissures, fistulas, and abscesses are common in Crohn's disease.
Complications:
Crohn's can lead to serious complications, including:
![]() Strictures: Chronic inflammation can cause scarring and narrowing (strictures) of the intestine, leading to bowel obstruction.
Strictures: Chronic inflammation can cause scarring and narrowing (strictures) of the intestine, leading to bowel obstruction.
![]() Fistulas: Abnormal connections between the intestine and other organs (e.g., bladder, vagina, skin) can form.
Fistulas: Abnormal connections between the intestine and other organs (e.g., bladder, vagina, skin) can form.
![]() Abscesses: Collections of pus can develop in the abdomen or around the anus.
Abscesses: Collections of pus can develop in the abdomen or around the anus.
![]() Malnutrition: Difficulty absorbing nutrients can lead to deficiencies.
Malnutrition: Difficulty absorbing nutrients can lead to deficiencies.
![]() Anemia: Due to blood loss and/or poor iron absorption.
Anemia: Due to blood loss and/or poor iron absorption.
![]() Colon cancer: People with Crohn's disease have an increased risk of colon cancer.
Colon cancer: People with Crohn's disease have an increased risk of colon cancer.
![]() Extraintestinal manifestations: Inflammation can affect other parts of the body, leading to joint pain (arthritis), skin problems (erythema nodosum, pyoderma gangrenosum), eye inflammation (uveitis), and liver problems.
Extraintestinal manifestations: Inflammation can affect other parts of the body, leading to joint pain (arthritis), skin problems (erythema nodosum, pyoderma gangrenosum), eye inflammation (uveitis), and liver problems.
Causes:
The exact cause of Crohn's disease is unknown, but it is believed to be a combination of factors:
![]() Genetics: Crohn's tends to run in families, suggesting a genetic component. Several genes have been linked to increased risk.
Genetics: Crohn's tends to run in families, suggesting a genetic component. Several genes have been linked to increased risk.
![]() Immune system: The immune system mistakenly attacks the GI tract, leading to chronic inflammation.
Immune system: The immune system mistakenly attacks the GI tract, leading to chronic inflammation.
![]() Environmental factors: Diet, smoking, and other environmental factors may play a role in triggering or exacerbating Crohn's.
Environmental factors: Diet, smoking, and other environmental factors may play a role in triggering or exacerbating Crohn's.
![]() Gut microbiome: Imbalances in the gut bacteria may contribute to the disease.
Gut microbiome: Imbalances in the gut bacteria may contribute to the disease.
Diagnosis:
Diagnosis typically involves:
![]() Medical history and physical exam:
Medical history and physical exam:
![]() Blood tests: To check for inflammation, anemia, and nutrient deficiencies.
Blood tests: To check for inflammation, anemia, and nutrient deficiencies.
![]() Stool tests: To rule out infections and check for blood.
Stool tests: To rule out infections and check for blood.
![]() Endoscopy (colonoscopy and/or upper endoscopy): A flexible tube with a camera is used to visualize the GI tract and take biopsies (tissue samples). This is a crucial part of the diagnosis.
Endoscopy (colonoscopy and/or upper endoscopy): A flexible tube with a camera is used to visualize the GI tract and take biopsies (tissue samples). This is a crucial part of the diagnosis.
![]() Imaging studies (CT scan, MRI): To assess the extent of inflammation and look for complications like strictures or fistulas.
Imaging studies (CT scan, MRI): To assess the extent of inflammation and look for complications like strictures or fistulas.
![]() Capsule endoscopy: A small camera is swallowed and takes pictures of the small intestine.
Capsule endoscopy: A small camera is swallowed and takes pictures of the small intestine.
Treatment:
There is no cure for Crohn's disease, but treatment aims to:
![]() Reduce inflammation: Medications are used to suppress the immune system and reduce inflammation.
Reduce inflammation: Medications are used to suppress the immune system and reduce inflammation.
![]() Relieve symptoms: Medications can help manage diarrhea, pain, and other symptoms.
Relieve symptoms: Medications can help manage diarrhea, pain, and other symptoms.
![]() Prevent complications: Treatment can help prevent strictures, fistulas, and other complications.
Prevent complications: Treatment can help prevent strictures, fistulas, and other complications.
![]() Maintain remission: The goal is to keep the disease under control and prevent flares (periods of active symptoms).
Maintain remission: The goal is to keep the disease under control and prevent flares (periods of active symptoms).
Common treatments include:
![]() Aminosalicylates (5-ASAs): Such as mesalamine, are used to reduce inflammation, especially in mild to moderate cases.
Aminosalicylates (5-ASAs): Such as mesalamine, are used to reduce inflammation, especially in mild to moderate cases.
![]() Corticosteroids: Such as prednisone, are powerful anti-inflammatory drugs used to treat acute flares. However, they have significant side effects and are not typically used for long-term maintenance.
Corticosteroids: Such as prednisone, are powerful anti-inflammatory drugs used to treat acute flares. However, they have significant side effects and are not typically used for long-term maintenance.
![]() Immunomodulators: Such as azathioprine and 6-mercaptopurine, suppress the immune system and are used to maintain remission.
Immunomodulators: Such as azathioprine and 6-mercaptopurine, suppress the immune system and are used to maintain remission.
![]() Biologic therapies: Such as anti-TNF agents (infliximab, adalimumab), anti-integrin agents (vedolizumab), and anti-IL-12/23 agents (ustekinumab), target specific parts of the immune system to reduce inflammation. These are often used for more severe cases or when other treatments have failed.
Biologic therapies: Such as anti-TNF agents (infliximab, adalimumab), anti-integrin agents (vedolizumab), and anti-IL-12/23 agents (ustekinumab), target specific parts of the immune system to reduce inflammation. These are often used for more severe cases or when other treatments have failed.
![]() Small molecule drugs: Such as tofacitinib, are oral medications that also target the immune system.
Small molecule drugs: Such as tofacitinib, are oral medications that also target the immune system.
![]() Antibiotics: May be used to treat infections or complications like abscesses.
Antibiotics: May be used to treat infections or complications like abscesses.
![]() Nutritional therapy: A special diet may be recommended to help manage symptoms and improve nutrition.
Nutritional therapy: A special diet may be recommended to help manage symptoms and improve nutrition.
![]() Surgery: May be necessary to treat complications such as strictures, fistulas, or abscesses. It's important to note that surgery doesn't cure Crohn's, and the disease can recur in other areas of the GI tract.
Surgery: May be necessary to treat complications such as strictures, fistulas, or abscesses. It's important to note that surgery doesn't cure Crohn's, and the disease can recur in other areas of the GI tract.
Management:
Crohn's disease is a chronic condition that requires ongoing management. Regular follow-up with a gastroenterologist is essential to monitor the disease and adjust treatment as needed. Lifestyle modifications, such as diet and stress management, can also play a role in managing the condition. Smoking cessation is strongly recommended as smoking worsens Crohn's.
In summary, Crohn's Disease is a complex and chronic inflammatory bowel disease that affects the digestive tract. It's characterized by inflammation, which can lead to a wide range of symptoms and complications. Treatment focuses on reducing inflammation, managing symptoms, preventing complications, and maintaining remission.