Deep Vein Thrombosis (Vascular Disease)
Published: 18 Jun 2025
ICD9: 453.40 ICD10: I82.409 ICD11: BD71
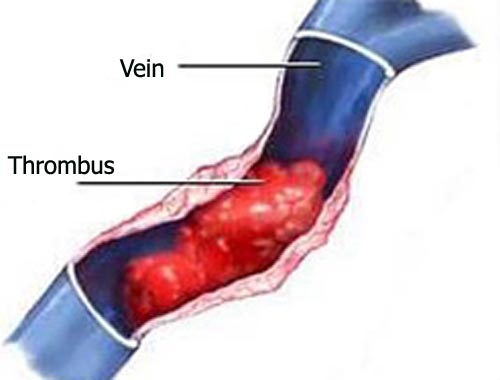
Deep Vein Thrombosis (DVT) is a serious condition that falls under the umbrella of vascular diseases.
Here's a breakdown:
What it is:
![]() Deep Veins: These are the large veins located deep within the body, usually in the legs but can also occur in the arms or, less commonly, in other parts of the body.
Deep Veins: These are the large veins located deep within the body, usually in the legs but can also occur in the arms or, less commonly, in other parts of the body.
![]() Thrombosis: This refers to the formation of a blood clot (thrombus) inside a blood vessel.
Thrombosis: This refers to the formation of a blood clot (thrombus) inside a blood vessel.
![]() Deep Vein Thrombosis (DVT) specifically means: A blood clot forms in one or more of these deep veins.
Deep Vein Thrombosis (DVT) specifically means: A blood clot forms in one or more of these deep veins.
Why it's a problem:
![]() Blockage of Blood Flow: The clot can partially or completely block the flow of blood through the vein. This can cause:
Blockage of Blood Flow: The clot can partially or completely block the flow of blood through the vein. This can cause:![]()

![]() Pain and Swelling: Especially in the affected limb.
Pain and Swelling: Especially in the affected limb.![]()

![]() Skin Discoloration: The leg may appear red, purple, or bluish.
Skin Discoloration: The leg may appear red, purple, or bluish.![]()

![]() Warmth: The affected area might feel warmer than the surrounding skin.
Warmth: The affected area might feel warmer than the surrounding skin.
![]() Pulmonary Embolism (PE): This is the *most dangerous* complication of DVT. If the clot, or a piece of it, breaks loose and travels through the bloodstream to the lungs, it can get lodged in a pulmonary artery (an artery carrying blood to the lungs). This blockage is called a pulmonary embolism, and it can:
Pulmonary Embolism (PE): This is the *most dangerous* complication of DVT. If the clot, or a piece of it, breaks loose and travels through the bloodstream to the lungs, it can get lodged in a pulmonary artery (an artery carrying blood to the lungs). This blockage is called a pulmonary embolism, and it can:![]()

![]() Damage the Lungs: Restricting blood flow.
Damage the Lungs: Restricting blood flow.![]()

![]() Strain the Heart: As the heart has to work harder to pump blood through the blocked arteries.
Strain the Heart: As the heart has to work harder to pump blood through the blocked arteries.![]()

![]() Be Life-Threatening: PE can cause shortness of breath, chest pain, lightheadedness, and even sudden death.
Be Life-Threatening: PE can cause shortness of breath, chest pain, lightheadedness, and even sudden death.
Causes and Risk Factors:
DVT can develop when something damages or slows blood flow in a vein. Common risk factors include:
![]() Prolonged immobility: Sitting or lying down for long periods, such as during long flights or car rides, bed rest after surgery, or paralysis.
Prolonged immobility: Sitting or lying down for long periods, such as during long flights or car rides, bed rest after surgery, or paralysis.
![]() Surgery: Especially hip, knee, or abdominal surgery.
Surgery: Especially hip, knee, or abdominal surgery.
![]() Trauma: Injuries to the veins, such as fractures.
Trauma: Injuries to the veins, such as fractures.
![]() Medical Conditions:
Medical Conditions:![]()

![]() Cancer
Cancer![]()

![]() Heart failure
Heart failure![]()

![]() Inflammatory bowel disease (IBD)
Inflammatory bowel disease (IBD)![]()

![]() Certain genetic disorders (e.g., Factor V Leiden)
Certain genetic disorders (e.g., Factor V Leiden)
![]() Medications:
Medications:![]()

![]() Birth control pills (especially those containing estrogen)
Birth control pills (especially those containing estrogen)![]()

![]() Hormone replacement therapy (HRT)
Hormone replacement therapy (HRT)
![]() Pregnancy: Increases the risk due to hormonal changes and pressure on the veins in the pelvis.
Pregnancy: Increases the risk due to hormonal changes and pressure on the veins in the pelvis.
![]() Obesity:
Obesity:
![]() Smoking:
Smoking:
![]() Age: Risk increases with age (over 60).
Age: Risk increases with age (over 60).
![]() Previous DVT or PE: Having had a clot before increases the likelihood of future clots.
Previous DVT or PE: Having had a clot before increases the likelihood of future clots.
![]() Family history: A family history of blood clots can increase risk.
Family history: A family history of blood clots can increase risk.
Symptoms:
DVT symptoms can vary, and some people may not have any noticeable symptoms. Common symptoms include:
![]() Swelling: Usually in one leg (rarely both).
Swelling: Usually in one leg (rarely both).
![]() Pain: Leg pain that often starts in the calf and feels like cramping or soreness.
Pain: Leg pain that often starts in the calf and feels like cramping or soreness.
![]() Warmth: The skin of the affected leg may feel warm to the touch.
Warmth: The skin of the affected leg may feel warm to the touch.
![]() Skin discoloration: Redness or a bluish or whitish tint.
Skin discoloration: Redness or a bluish or whitish tint.
![]() Sometimes, enlarged superficial veins
Sometimes, enlarged superficial veins
![]() Note: Symptoms may not be severe*
Note: Symptoms may not be severe*
Diagnosis:
![]() Physical Exam: The doctor will examine the legs and ask about medical history and risk factors.
Physical Exam: The doctor will examine the legs and ask about medical history and risk factors.
![]() Duplex Ultrasound: This is the most common test. It uses sound waves to create images of the veins and check blood flow.
Duplex Ultrasound: This is the most common test. It uses sound waves to create images of the veins and check blood flow.
![]() Venography: An X-ray of the veins after injecting a contrast dye. This is less common now, as ultrasound is usually sufficient.
Venography: An X-ray of the veins after injecting a contrast dye. This is less common now, as ultrasound is usually sufficient.
![]() D-dimer blood test: Measures a substance released when a blood clot breaks down. A negative result makes a DVT less likely, but a positive result requires further testing.
D-dimer blood test: Measures a substance released when a blood clot breaks down. A negative result makes a DVT less likely, but a positive result requires further testing.
Treatment:
The main goals of treatment are to:
![]() Stop the clot from getting bigger.
Stop the clot from getting bigger.
![]() Prevent the clot from breaking loose and traveling to the lungs (prevent PE).
Prevent the clot from breaking loose and traveling to the lungs (prevent PE).
![]() Reduce the risk of future clots.
Reduce the risk of future clots.
Treatment options include:
![]() Anticoagulants (Blood Thinners): These medications prevent blood clots from forming or growing larger. Common options include:
Anticoagulants (Blood Thinners): These medications prevent blood clots from forming or growing larger. Common options include:![]()

![]() Heparin (given by injection or IV)
Heparin (given by injection or IV)![]()

![]() Warfarin (Coumadin) – an older oral medication that requires regular blood monitoring.
Warfarin (Coumadin) – an older oral medication that requires regular blood monitoring.![]()

![]() Direct oral anticoagulants (DOACs) such as rivaroxaban (Xarelto), apixaban (Eliquis), edoxaban (Savaysa), and dabigatran (Pradaxa). These are typically preferred over warfarin due to ease of use and less need for monitoring.
Direct oral anticoagulants (DOACs) such as rivaroxaban (Xarelto), apixaban (Eliquis), edoxaban (Savaysa), and dabigatran (Pradaxa). These are typically preferred over warfarin due to ease of use and less need for monitoring.
![]() Thrombolytics (Clot Busters): These medications can dissolve the clot quickly, but they are used less frequently due to a higher risk of bleeding. They are reserved for severe cases of DVT or PE.
Thrombolytics (Clot Busters): These medications can dissolve the clot quickly, but they are used less frequently due to a higher risk of bleeding. They are reserved for severe cases of DVT or PE.
![]() Compression Stockings: These elastic stockings help reduce swelling and improve blood flow in the legs. They are worn daily.
Compression Stockings: These elastic stockings help reduce swelling and improve blood flow in the legs. They are worn daily.
![]() Inferior Vena Cava (IVC) Filter: A small filter is placed in the inferior vena cava (the large vein that carries blood from the legs to the heart) to trap clots before they can reach the lungs. This is typically used if someone cannot take anticoagulants or if anticoagulants are not working.
Inferior Vena Cava (IVC) Filter: A small filter is placed in the inferior vena cava (the large vein that carries blood from the legs to the heart) to trap clots before they can reach the lungs. This is typically used if someone cannot take anticoagulants or if anticoagulants are not working.
![]() Thrombectomy: A surgical procedure to remove the clot from the vein. This is less common but may be considered in certain situations.
Thrombectomy: A surgical procedure to remove the clot from the vein. This is less common but may be considered in certain situations.
Prevention:
Preventing DVT is crucial, especially for people at high risk. Strategies include:
![]() Movement: Avoid prolonged immobility. Take breaks to walk around during long trips. Do leg exercises while sitting.
Movement: Avoid prolonged immobility. Take breaks to walk around during long trips. Do leg exercises while sitting.
![]() Compression Stockings: Wear compression stockings, especially during long periods of sitting or standing.
Compression Stockings: Wear compression stockings, especially during long periods of sitting or standing.
![]() Hydration: Drink plenty of fluids to keep the blood from becoming too thick.
Hydration: Drink plenty of fluids to keep the blood from becoming too thick.
![]() Weight Management: Maintain a healthy weight.
Weight Management: Maintain a healthy weight.
![]() Smoking Cessation: Quit smoking.
Smoking Cessation: Quit smoking.
![]() Anticoagulation (Prophylactic): Doctors may prescribe blood thinners before or after surgery, or during prolonged periods of immobility, to prevent clots.
Anticoagulation (Prophylactic): Doctors may prescribe blood thinners before or after surgery, or during prolonged periods of immobility, to prevent clots.
![]() Elevate your legs: This is especially beneficial when seated.
Elevate your legs: This is especially beneficial when seated.
In summary, Deep Vein Thrombosis is a serious vascular condition where a blood clot forms in a deep vein, often in the leg. It can lead to significant complications, including pulmonary embolism, and requires prompt diagnosis and treatment. Prevention is key, especially for individuals with risk factors.
Disclaimer: This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment. If you suspect you may have DVT, seek immediate medical attention.