Diabetic ketoacidosis
Published: 18 Jun 2025
ICD9: 250.1 ICD10: E10.10 ICD11: 5A22
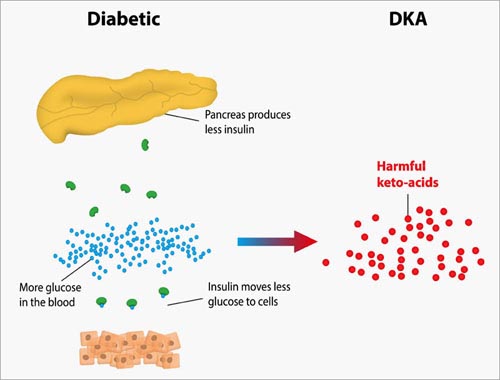
Diabetic ketoacidosis (DKA) is a serious complication of diabetes that occurs when your body produces high levels of blood acids called ketones.
It's most common in people with type 1 diabetes, but can also occur in people with type 2 diabetes.
In simpler terms:
Imagine your body needs fuel (glucose/sugar) to function. Insulin is like a key that unlocks cells to allow glucose to enter. In DKA, either there's not enough insulin (type 1 diabetes) or the insulin isn't working properly (type 2 diabetes), so glucose can't get into the cells. As a result, the body starts breaking down fat for energy. This process produces ketones, which are acidic chemicals. When ketones build up too much in the blood, it leads to DKA.
Here's a breakdown of the key aspects:
![]() Diabetes: DKA is almost always associated with diabetes, either diagnosed or undiagnosed.
Diabetes: DKA is almost always associated with diabetes, either diagnosed or undiagnosed.
![]() Insulin Deficiency: The underlying problem is usually a lack of insulin or insulin resistance.
Insulin Deficiency: The underlying problem is usually a lack of insulin or insulin resistance.
![]() Ketones: When the body can't use glucose for energy, it breaks down fat, producing ketones.
Ketones: When the body can't use glucose for energy, it breaks down fat, producing ketones.
![]() Acidosis: An excessive build-up of ketones makes the blood acidic (ketoacidosis).
Acidosis: An excessive build-up of ketones makes the blood acidic (ketoacidosis).
![]() Dehydration: High blood sugar leads to increased urination, causing dehydration.
Dehydration: High blood sugar leads to increased urination, causing dehydration.
Causes:
![]() Missed or insufficient insulin doses: This is a common cause, especially in people with type 1 diabetes.
Missed or insufficient insulin doses: This is a common cause, especially in people with type 1 diabetes.
![]() Illness: Infections, such as pneumonia or urinary tract infections, can increase the body's demand for insulin.
Illness: Infections, such as pneumonia or urinary tract infections, can increase the body's demand for insulin.
![]() Stress: Physical or emotional stress can affect blood sugar levels.
Stress: Physical or emotional stress can affect blood sugar levels.
![]() Surgery or trauma: These can also increase the body's demand for insulin.
Surgery or trauma: These can also increase the body's demand for insulin.
![]() Certain medications: Steroids can raise blood sugar levels.
Certain medications: Steroids can raise blood sugar levels.
![]() Undiagnosed diabetes: Sometimes DKA is the first sign of diabetes.
Undiagnosed diabetes: Sometimes DKA is the first sign of diabetes.
![]() Problems with insulin pump: Blocked or malfunctioning insulin pump can lead to insulin deficiency.
Problems with insulin pump: Blocked or malfunctioning insulin pump can lead to insulin deficiency.
Symptoms:
DKA symptoms usually develop quickly, over a period of 24 hours, but sometimes they can take longer. They include:
![]() Excessive thirst: You feel very thirsty, even after drinking.
Excessive thirst: You feel very thirsty, even after drinking.
![]() Frequent urination: You need to pee often.
Frequent urination: You need to pee often.
![]() Nausea and vomiting: Feeling sick to your stomach.
Nausea and vomiting: Feeling sick to your stomach.
![]() Stomach pain: Abdominal pain.
Stomach pain: Abdominal pain.
![]() Weakness or fatigue: Feeling tired and weak.
Weakness or fatigue: Feeling tired and weak.
![]() Fruity-scented breath: A distinct, sweet smell on the breath, like nail polish remover or overripe fruit (due to acetone, a type of ketone).
Fruity-scented breath: A distinct, sweet smell on the breath, like nail polish remover or overripe fruit (due to acetone, a type of ketone).
![]() Rapid, deep breathing (Kussmaul breathing): The body tries to expel the acid.
Rapid, deep breathing (Kussmaul breathing): The body tries to expel the acid.
![]() Confusion or difficulty concentrating: Can progress to drowsiness and coma.
Confusion or difficulty concentrating: Can progress to drowsiness and coma.
![]() High blood sugar levels: Usually significantly elevated (often above 250 mg/dL, but it can vary).
High blood sugar levels: Usually significantly elevated (often above 250 mg/dL, but it can vary).
![]() Ketones in the urine or blood: Detected with ketone strips or blood ketone meters.
Ketones in the urine or blood: Detected with ketone strips or blood ketone meters.
Diagnosis:
DKA is diagnosed based on:
![]() Blood sugar levels: Elevated blood glucose levels.
Blood sugar levels: Elevated blood glucose levels.
![]() Blood ketone levels: High levels of ketones in the blood.
Blood ketone levels: High levels of ketones in the blood.
![]() Arterial blood gas (ABG): Measures the acidity (pH) of the blood. In DKA, the blood will be acidic.
Arterial blood gas (ABG): Measures the acidity (pH) of the blood. In DKA, the blood will be acidic.
![]() Electrolyte levels: Can be imbalanced due to dehydration and other factors.
Electrolyte levels: Can be imbalanced due to dehydration and other factors.
![]() Urinalysis: Checks for glucose and ketones in the urine.
Urinalysis: Checks for glucose and ketones in the urine.
Treatment:
DKA is a medical emergency and requires immediate hospital treatment. Treatment typically involves:
![]() Insulin: Administered intravenously (IV) to help glucose enter cells.
Insulin: Administered intravenously (IV) to help glucose enter cells.
![]() Fluids: IV fluids to correct dehydration.
Fluids: IV fluids to correct dehydration.
![]() Electrolyte replacement: Replenishing electrolytes like potassium, sodium, and phosphate, which are often lost during DKA.
Electrolyte replacement: Replenishing electrolytes like potassium, sodium, and phosphate, which are often lost during DKA.
![]() Monitoring: Close monitoring of blood sugar, ketone levels, electrolytes, and other vital signs.
Monitoring: Close monitoring of blood sugar, ketone levels, electrolytes, and other vital signs.
![]() Identifying and treating the underlying cause: Addressing the reason why DKA occurred (e.g., treating an infection).
Identifying and treating the underlying cause: Addressing the reason why DKA occurred (e.g., treating an infection).
Prevention:
Preventing DKA involves:
![]() Careful diabetes management: Following your doctor's instructions regarding insulin, diet, and exercise.
Careful diabetes management: Following your doctor's instructions regarding insulin, diet, and exercise.
![]() Monitoring blood sugar regularly: Checking blood sugar levels frequently, especially when you are sick.
Monitoring blood sugar regularly: Checking blood sugar levels frequently, especially when you are sick.
![]() Checking for ketones: If your blood sugar is high or you are feeling unwell, check your urine or blood for ketones.
Checking for ketones: If your blood sugar is high or you are feeling unwell, check your urine or blood for ketones.
![]() Never skipping insulin doses: Even when you're sick, you usually still need some insulin. Talk to your doctor about sick-day management.
Never skipping insulin doses: Even when you're sick, you usually still need some insulin. Talk to your doctor about sick-day management.
![]() Sick-day management: Having a plan in place for what to do when you are sick, including adjusting insulin doses and monitoring blood sugar and ketones more frequently.
Sick-day management: Having a plan in place for what to do when you are sick, including adjusting insulin doses and monitoring blood sugar and ketones more frequently.
![]() Education: Understanding diabetes, insulin, and the signs and symptoms of DKA.
Education: Understanding diabetes, insulin, and the signs and symptoms of DKA.
Important Note: DKA is a life-threatening condition. If you suspect you or someone you know has DKA, seek immediate medical attention. Do not try to treat it at home. Call emergency services (911 in the US) or go to the nearest emergency room.