Diverticulosis (Diverticulitis, Diverticular disease)
Published: 18 Jun 2025
ICD9: 562.10 ICD10: K57.30 ICD11: DD00
Let's break down diverticulosis, diverticulitis, and diverticular disease:
Diverticulosis
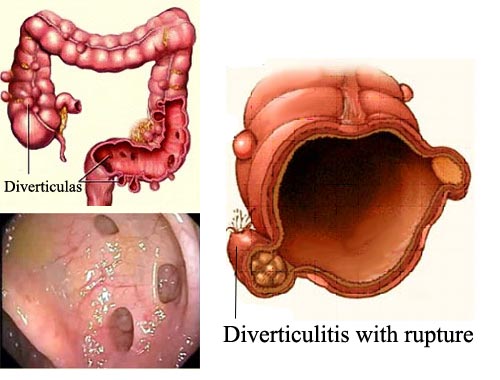
![]() What it is: This is the *presence* of small pouches or sacs called diverticula that develop in the wall of the colon (large intestine).
What it is: This is the *presence* of small pouches or sacs called diverticula that develop in the wall of the colon (large intestine).
Think of them like little hernias in the lining of the colon.
![]() How it happens: Increased pressure within the colon can cause the inner lining to push through weak spots in the outer muscle layer. This pressure can be caused by things like:
How it happens: Increased pressure within the colon can cause the inner lining to push through weak spots in the outer muscle layer. This pressure can be caused by things like:![]()

![]() Low-fiber diet (common culprit)
Low-fiber diet (common culprit)![]()

![]() Straining during bowel movements
Straining during bowel movements![]()

![]() Age (more common as people get older)
Age (more common as people get older)![]()

![]() Changes in gut bacteria
Changes in gut bacteria
![]() Symptoms: Most people with diverticulosis have NO symptoms. It's often discovered during a routine colonoscopy or other test. When symptoms do occur, they can include:
Symptoms: Most people with diverticulosis have NO symptoms. It's often discovered during a routine colonoscopy or other test. When symptoms do occur, they can include:![]()

![]() Mild cramping
Mild cramping![]()

![]() Bloating
Bloating![]()

![]() Constipation
Constipation![]()

![]() Less commonly, diarrhea.
Less commonly, diarrhea.
![]() Important Note: Diverticulosis is common, especially with increasing age. Having diverticulosis does NOT mean you will automatically develop diverticulitis.
Important Note: Diverticulosis is common, especially with increasing age. Having diverticulosis does NOT mean you will automatically develop diverticulitis.
Diverticulitis
![]() What it is: This is inflammation or infection of one or more diverticula. It happens when a diverticulum becomes blocked (by stool, for example) and bacteria start to grow, leading to infection and inflammation.
What it is: This is inflammation or infection of one or more diverticula. It happens when a diverticulum becomes blocked (by stool, for example) and bacteria start to grow, leading to infection and inflammation.
![]() Symptoms: Diverticulitis symptoms can vary in severity, but they often include:
Symptoms: Diverticulitis symptoms can vary in severity, but they often include:![]()

![]() Abdominal pain: Typically in the lower left side of the abdomen, but it can be on the right or elsewhere. The pain can be sudden or gradually worsen over a few days.
Abdominal pain: Typically in the lower left side of the abdomen, but it can be on the right or elsewhere. The pain can be sudden or gradually worsen over a few days.![]()

![]() Fever
Fever![]()

![]() Nausea and vomiting
Nausea and vomiting![]()

![]() Constipation or diarrhea
Constipation or diarrhea![]()

![]() Abdominal tenderness
Abdominal tenderness
![]() Complications: If left untreated, diverticulitis can lead to serious complications, including:
Complications: If left untreated, diverticulitis can lead to serious complications, including:![]()

![]() Abscess: A collection of pus within the diverticulum or surrounding tissue.
Abscess: A collection of pus within the diverticulum or surrounding tissue.![]()

![]() Perforation: A hole or tear in the colon wall, which can leak bacteria into the abdominal cavity (peritonitis).
Perforation: A hole or tear in the colon wall, which can leak bacteria into the abdominal cavity (peritonitis).![]()

![]() Fistula: An abnormal connection between the colon and another organ (like the bladder or vagina).
Fistula: An abnormal connection between the colon and another organ (like the bladder or vagina).![]()

![]() Stricture: Narrowing of the colon due to scarring from repeated inflammation.
Stricture: Narrowing of the colon due to scarring from repeated inflammation.![]()

![]() Bleeding: Diverticular bleeding is another complication.
Bleeding: Diverticular bleeding is another complication.
![]() Treatment: Treatment for diverticulitis depends on the severity of the symptoms. It can range from antibiotics and a liquid diet for mild cases to hospitalization, IV antibiotics, and possibly surgery for severe cases with complications.
Treatment: Treatment for diverticulitis depends on the severity of the symptoms. It can range from antibiotics and a liquid diet for mild cases to hospitalization, IV antibiotics, and possibly surgery for severe cases with complications.
Diverticular Disease
![]() What it is: This is a broad term that encompasses both diverticulosis and diverticulitis, as well as other conditions related to diverticula. It's used when discussing the overall spectrum of problems associated with these pouches.
What it is: This is a broad term that encompasses both diverticulosis and diverticulitis, as well as other conditions related to diverticula. It's used when discussing the overall spectrum of problems associated with these pouches.
Think of it this way:
![]() Diverticulosis: The *condition* of having diverticula (pouches) in the colon.
Diverticulosis: The *condition* of having diverticula (pouches) in the colon.
![]() Diverticulitis: An *inflammation/infection* of those pouches.
Diverticulitis: An *inflammation/infection* of those pouches.
![]() Diverticular Disease: The *umbrella term* for all conditions related to diverticula.
Diverticular Disease: The *umbrella term* for all conditions related to diverticula.
Risk factors:
![]() Age: The risk increases with age.
Age: The risk increases with age.
![]() Low-fiber diet: A major contributing factor.
Low-fiber diet: A major contributing factor.
![]() Obesity
Obesity
![]() Lack of exercise
Lack of exercise
![]() Smoking
Smoking
![]() Certain medications: NSAIDs (like ibuprofen) and steroids.
Certain medications: NSAIDs (like ibuprofen) and steroids.
![]() Genetics: There may be a genetic predisposition.
Genetics: There may be a genetic predisposition.
Diagnosis:
![]() Physical exam: A doctor will examine your abdomen.
Physical exam: A doctor will examine your abdomen.
![]() Imaging tests:
Imaging tests:![]()

![]() CT scan: The most common and accurate test to diagnose diverticulitis.
CT scan: The most common and accurate test to diagnose diverticulitis.![]()

![]() Colonoscopy: Used to visualize the colon, especially after an episode of diverticulitis has resolved (to rule out other problems). Generally avoided during acute diverticulitis.
Colonoscopy: Used to visualize the colon, especially after an episode of diverticulitis has resolved (to rule out other problems). Generally avoided during acute diverticulitis.![]()

![]() Flexible sigmoidoscopy: Similar to colonoscopy, but only examines the lower part of the colon.
Flexible sigmoidoscopy: Similar to colonoscopy, but only examines the lower part of the colon.
![]() Blood tests: To check for signs of infection.
Blood tests: To check for signs of infection.
Prevention:
![]() High-fiber diet: The most important thing! Aim for 25-35 grams of fiber per day from fruits, vegetables, whole grains, and legumes.
High-fiber diet: The most important thing! Aim for 25-35 grams of fiber per day from fruits, vegetables, whole grains, and legumes.
![]() Drink plenty of water: Helps move fiber through the digestive system.
Drink plenty of water: Helps move fiber through the digestive system.
![]() Regular exercise
Regular exercise
![]() Maintain a healthy weight
Maintain a healthy weight
![]() Avoid smoking
Avoid smoking
In summary: Diverticulosis is the *presence* of pouches in the colon. Diverticulitis is when those pouches become *inflamed or infected*. A high-fiber diet is key for prevention. If you suspect you have diverticulitis, see a doctor promptly.