Endometriosis
Published: 18 Jun 2025
ICD9: 617.9 ICD10: N80.9 ICD11: GA10
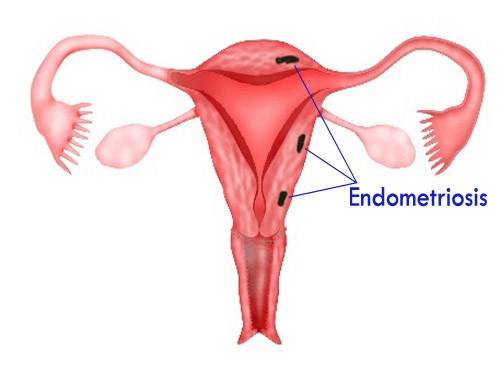
Endometriosis is a condition where tissue similar to the lining of the uterus (the endometrium) grows outside of the uterus.
This misplaced tissue can be found in various locations within the body, but it's most commonly found in the:
![]() Ovaries: Where it can form cysts called endometriomas.
Ovaries: Where it can form cysts called endometriomas.
![]() Fallopian Tubes: Potentially causing blockage and affecting fertility.
Fallopian Tubes: Potentially causing blockage and affecting fertility.
![]() Outer surface of the Uterus
Outer surface of the Uterus
![]() Ligaments supporting the Uterus
Ligaments supporting the Uterus
![]() Bowel
Bowel
![]() Bladder
Bladder
In rare cases, it can also be found in more distant locations like the lungs or brain.
How it Works:
This endometrial-like tissue outside the uterus still responds to hormonal changes during the menstrual cycle. It thickens, breaks down, and bleeds, just like the uterine lining. However, because this blood and tissue have no way to exit the body, it can cause:
![]() Inflammation: The surrounding tissues become irritated and inflamed.
Inflammation: The surrounding tissues become irritated and inflamed.
![]() Scar Tissue (Adhesions): This scar tissue can bind organs together, causing pain and dysfunction.
Scar Tissue (Adhesions): This scar tissue can bind organs together, causing pain and dysfunction.
![]() Pain: The misplaced tissue, bleeding, and inflammation all contribute to pain.
Pain: The misplaced tissue, bleeding, and inflammation all contribute to pain.
![]() Infertility: Endometriosis can affect fertility by damaging the ovaries, fallopian tubes, or interfering with implantation.
Infertility: Endometriosis can affect fertility by damaging the ovaries, fallopian tubes, or interfering with implantation.
Symptoms of Endometriosis:
The most common symptom is pelvic pain, often associated with menstruation. However, the severity of pain doesn't always correlate with the extent of the endometriosis. Some women with mild endometriosis experience debilitating pain, while others with more extensive disease have few symptoms. Other common symptoms include:
![]() Painful periods (dysmenorrhea): Severe cramps that may start before and last for several days during a period.
Painful periods (dysmenorrhea): Severe cramps that may start before and last for several days during a period.
![]() Pain with intercourse (dyspareunia): Pain during or after sexual activity.
Pain with intercourse (dyspareunia): Pain during or after sexual activity.
![]() Pain with bowel movements or urination: Especially during a period.
Pain with bowel movements or urination: Especially during a period.
![]() Heavy bleeding or bleeding between periods (menorrhagia/metrorrhagia): Abnormally heavy or prolonged menstrual flow, or bleeding between periods.
Heavy bleeding or bleeding between periods (menorrhagia/metrorrhagia): Abnormally heavy or prolonged menstrual flow, or bleeding between periods.
![]() Infertility: Difficulty getting pregnant.
Infertility: Difficulty getting pregnant.
![]() Fatigue: Persistent and unexplained tiredness.
Fatigue: Persistent and unexplained tiredness.
![]() Bloating, nausea, constipation, or diarrhea: Especially during a period.
Bloating, nausea, constipation, or diarrhea: Especially during a period.
Causes and Risk Factors:
The exact cause of endometriosis isn't fully understood, but several theories exist:
![]() Retrograde Menstruation: Menstrual blood containing endometrial cells flows backward through the fallopian tubes and into the pelvic cavity.
Retrograde Menstruation: Menstrual blood containing endometrial cells flows backward through the fallopian tubes and into the pelvic cavity.
![]() Immune System Dysfunction: A problem with the immune system may allow endometrial cells to grow outside the uterus.
Immune System Dysfunction: A problem with the immune system may allow endometrial cells to grow outside the uterus.
![]() Metaplasia: Cells outside the uterus transform into endometrial-like cells.
Metaplasia: Cells outside the uterus transform into endometrial-like cells.
![]() Surgical Scar Implantation: After surgeries like hysterectomy or C-section, endometrial cells may attach to surgical incisions.
Surgical Scar Implantation: After surgeries like hysterectomy or C-section, endometrial cells may attach to surgical incisions.
![]() Genetic Factors: There's evidence that endometriosis can run in families.
Genetic Factors: There's evidence that endometriosis can run in families.
Risk factors include:
![]() Family history of endometriosis
Family history of endometriosis
![]() Never having children
Never having children
![]() Starting your period at an early age
Starting your period at an early age
![]() Short menstrual cycles (less than 27 days)
Short menstrual cycles (less than 27 days)
![]() Heavy menstrual periods
Heavy menstrual periods
![]() High levels of estrogen in the body
High levels of estrogen in the body
Diagnosis:
Diagnosing endometriosis can be challenging, as symptoms can mimic other conditions. The diagnostic process typically involves:
![]() Medical History and Physical Exam: The doctor will ask about your symptoms, menstrual history, and family history.
Medical History and Physical Exam: The doctor will ask about your symptoms, menstrual history, and family history.
![]() Pelvic Exam: To check for abnormalities in the pelvic organs.
Pelvic Exam: To check for abnormalities in the pelvic organs.
![]() Imaging Tests:
Imaging Tests:![]()

![]() Ultrasound: Can help identify endometriomas (cysts on the ovaries).
Ultrasound: Can help identify endometriomas (cysts on the ovaries).![]()

![]() MRI: Can provide a more detailed view of the pelvic organs and detect endometriosis lesions.
MRI: Can provide a more detailed view of the pelvic organs and detect endometriosis lesions.
![]() Laparoscopy: This is the *gold standard* for diagnosis. A small incision is made in the abdomen, and a thin, lighted tube (laparoscope) is inserted to visualize the pelvic organs and confirm the presence of endometriosis. Biopsies can be taken during laparoscopy to confirm the diagnosis under a microscope.
Laparoscopy: This is the *gold standard* for diagnosis. A small incision is made in the abdomen, and a thin, lighted tube (laparoscope) is inserted to visualize the pelvic organs and confirm the presence of endometriosis. Biopsies can be taken during laparoscopy to confirm the diagnosis under a microscope.
Treatment:
There is no cure for endometriosis, but treatments are available to manage the symptoms and improve quality of life. Treatment options depend on the severity of the symptoms, age, desire for future pregnancy, and overall health. Common treatments include:
![]() Pain Medication: Over-the-counter or prescription pain relievers to manage pain.
Pain Medication: Over-the-counter or prescription pain relievers to manage pain.
![]() Hormone Therapy:
Hormone Therapy:![]()

![]() Birth Control Pills: Help regulate hormone levels and reduce menstrual flow, often reducing pain and slowing the growth of endometriosis.
Birth Control Pills: Help regulate hormone levels and reduce menstrual flow, often reducing pain and slowing the growth of endometriosis.![]()

![]() Progestin Therapy: Can help suppress endometrial tissue growth.
Progestin Therapy: Can help suppress endometrial tissue growth.![]()

![]() GnRH Agonists and Antagonists: These medications temporarily lower estrogen levels, inducing a temporary menopause-like state, which can shrink endometriosis lesions and reduce pain.
GnRH Agonists and Antagonists: These medications temporarily lower estrogen levels, inducing a temporary menopause-like state, which can shrink endometriosis lesions and reduce pain.
![]() Surgery:
Surgery:![]()

![]() Laparoscopic Surgery: To remove or destroy endometriosis lesions and scar tissue. This can be done through excision (cutting out the lesions) or ablation (burning them).
Laparoscopic Surgery: To remove or destroy endometriosis lesions and scar tissue. This can be done through excision (cutting out the lesions) or ablation (burning them).![]()

![]() Hysterectomy: Removal of the uterus. This is usually a last resort for women who have severe symptoms and don't plan to have children. Hysterectomy alone may not cure endometriosis; the ovaries may need to be removed as well (oophorectomy) to stop estrogen production.
Hysterectomy: Removal of the uterus. This is usually a last resort for women who have severe symptoms and don't plan to have children. Hysterectomy alone may not cure endometriosis; the ovaries may need to be removed as well (oophorectomy) to stop estrogen production.
![]() Fertility Treatments: Women with endometriosis who want to get pregnant may need fertility treatments, such as in vitro fertilization (IVF).
Fertility Treatments: Women with endometriosis who want to get pregnant may need fertility treatments, such as in vitro fertilization (IVF).
Important Considerations:
![]() Endometriosis is a chronic condition, meaning it can last for many years.
Endometriosis is a chronic condition, meaning it can last for many years.
![]() Early diagnosis and treatment can help prevent the progression of the disease and improve quality of life.
Early diagnosis and treatment can help prevent the progression of the disease and improve quality of life.
![]() Living with endometriosis can be challenging, and many women benefit from support groups or counseling.
Living with endometriosis can be challenging, and many women benefit from support groups or counseling.
![]() Management is often individualized, and what works for one woman may not work for another.
Management is often individualized, and what works for one woman may not work for another.
If you suspect you have endometriosis, it's crucial to see a doctor for diagnosis and treatment. Don't hesitate to advocate for yourself and seek a specialist in endometriosis if necessary.