Epidural Hematoma
Published: 18 Jun 2025
ICD9: 852.4 ICD10: S06.4X0A ICD11: NA07.5
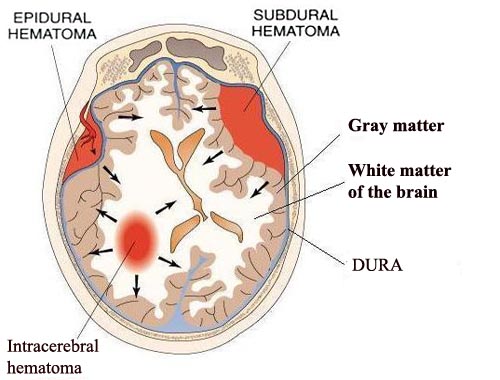
An epidural hematoma (EDH) is a collection of blood between the dura mater (the tough outer membrane covering the brain and spinal cord) and the skull.
Think of it as blood pooling *outside* the brain itself, but *inside* the skull.
Here's a breakdown:
![]() Epidural: "Epi" means "upon" or "above," and "dural" refers to the dura mater. So, epidural means "above the dura."
Epidural: "Epi" means "upon" or "above," and "dural" refers to the dura mater. So, epidural means "above the dura."
![]() Hematoma: A collection of blood outside of blood vessels.
Hematoma: A collection of blood outside of blood vessels.
Key Characteristics and Information:
![]() Cause: EDHs are almost always caused by a skull fracture that tears an underlying artery, most commonly the middle meningeal artery. This artery runs along the temporal bone (side of the head).
Cause: EDHs are almost always caused by a skull fracture that tears an underlying artery, most commonly the middle meningeal artery. This artery runs along the temporal bone (side of the head).
![]() Arterial Bleed: Because the bleeding is typically arterial, the hematoma develops quickly. This makes EDHs very dangerous and requires prompt diagnosis and treatment.
Arterial Bleed: Because the bleeding is typically arterial, the hematoma develops quickly. This makes EDHs very dangerous and requires prompt diagnosis and treatment.
![]() Classic Presentation (although not always present):
Classic Presentation (although not always present):![]()

![]() Brief Loss of Consciousness: The patient may be knocked out at the time of the injury.
Brief Loss of Consciousness: The patient may be knocked out at the time of the injury.![]()

![]() Lucid Interval: A period of time where the patient regains consciousness and seems relatively normal. This can last minutes to hours.
Lucid Interval: A period of time where the patient regains consciousness and seems relatively normal. This can last minutes to hours.![]()

![]() Rapid Neurological Deterioration: As the hematoma expands, it puts pressure on the brain, leading to worsening symptoms like headache, vomiting, confusion, weakness, seizures, and eventually coma.
Rapid Neurological Deterioration: As the hematoma expands, it puts pressure on the brain, leading to worsening symptoms like headache, vomiting, confusion, weakness, seizures, and eventually coma.
![]() Location: Most commonly found in the temporal region (side of the head), but can occur anywhere there's a skull fracture and an injured artery.
Location: Most commonly found in the temporal region (side of the head), but can occur anywhere there's a skull fracture and an injured artery.
![]() Shape on CT Scan: EDHs typically have a lens-shaped (or biconvex) appearance on CT scans. This is because the dura is tightly adherent to the skull at the sutures, limiting the spread of the blood. The hematoma is confined by the sutures, giving it that characteristic shape.
Shape on CT Scan: EDHs typically have a lens-shaped (or biconvex) appearance on CT scans. This is because the dura is tightly adherent to the skull at the sutures, limiting the spread of the blood. The hematoma is confined by the sutures, giving it that characteristic shape.
![]() Diagnosis: CT scan of the head is the primary diagnostic tool. MRI can also be used.
Diagnosis: CT scan of the head is the primary diagnostic tool. MRI can also be used.
![]() Treatment: Prompt surgical intervention is usually necessary. The goal is to evacuate the hematoma to relieve pressure on the brain. This may involve a craniotomy (removing a piece of the skull) or a burr hole (drilling a small hole in the skull).
Treatment: Prompt surgical intervention is usually necessary. The goal is to evacuate the hematoma to relieve pressure on the brain. This may involve a craniotomy (removing a piece of the skull) or a burr hole (drilling a small hole in the skull).
![]() Prognosis: The prognosis depends on several factors, including the size of the hematoma, the patient's overall health, and the speed of diagnosis and treatment. With rapid intervention, many patients can make a good recovery. However, delayed treatment can lead to permanent brain damage or death.
Prognosis: The prognosis depends on several factors, including the size of the hematoma, the patient's overall health, and the speed of diagnosis and treatment. With rapid intervention, many patients can make a good recovery. However, delayed treatment can lead to permanent brain damage or death.
In Summary: Epidural hematomas are serious and potentially life-threatening conditions resulting from bleeding between the skull and the dura mater, usually caused by a skull fracture damaging an artery. Rapid diagnosis and surgical intervention are crucial for a favorable outcome. The classic presentation is a period of unconsciousness followed by a lucid interval and then rapid neurological decline, but this doesn't always occur. The lens-shaped appearance on CT is a key diagnostic feature.