Gallstones (Cholelithiasis)
Published: 18 Jun 2025
ICD9: 574 ICD10: K80.00 ICD11: DC11.3
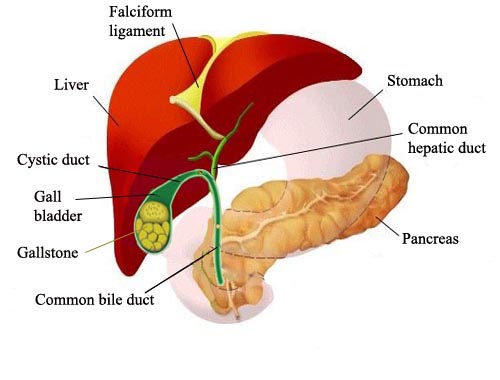
Gallstones, also known as cholelithiasis, are hard deposits that form inside the gallbladder.
The gallbladder is a small, pear-shaped organ located on the upper right side of your abdomen, just beneath your liver. Its main function is to store and concentrate bile, a digestive fluid produced by the liver that helps the body break down and absorb fats.
Here's a breakdown of key aspects of gallstones:
What they are:
![]() Solid concretions: Gallstones are solid, pebble-like substances made up of cholesterol, bilirubin (a pigment from broken-down red blood cells), and calcium salts.
Solid concretions: Gallstones are solid, pebble-like substances made up of cholesterol, bilirubin (a pigment from broken-down red blood cells), and calcium salts.
![]() Vary in size and number: They can range in size from tiny grains of sand to as large as golf balls. You can have one large gallstone or many small ones.
Vary in size and number: They can range in size from tiny grains of sand to as large as golf balls. You can have one large gallstone or many small ones.
Types of Gallstones:
![]() Cholesterol stones: These are the most common type (about 80% of cases). They are usually yellow-green in color and primarily made of hardened cholesterol.
Cholesterol stones: These are the most common type (about 80% of cases). They are usually yellow-green in color and primarily made of hardened cholesterol.
![]() Pigment stones: These are smaller, darker stones composed of bilirubin. They tend to develop in people with certain medical conditions, such as liver cirrhosis, biliary tract infections, or hereditary blood disorders (like sickle cell anemia) that cause the liver to make too much bilirubin.
Pigment stones: These are smaller, darker stones composed of bilirubin. They tend to develop in people with certain medical conditions, such as liver cirrhosis, biliary tract infections, or hereditary blood disorders (like sickle cell anemia) that cause the liver to make too much bilirubin.
![]() Mixed stones: These stones contain a combination of cholesterol, bilirubin, and calcium salts.
Mixed stones: These stones contain a combination of cholesterol, bilirubin, and calcium salts.
Causes and Risk Factors:
While the exact cause of gallstones isn't always clear, several factors can increase your risk:
![]() High cholesterol levels: Excess cholesterol in the bile can crystalize and form stones.
High cholesterol levels: Excess cholesterol in the bile can crystalize and form stones.
![]() High bilirubin levels: Conditions that cause the liver to produce more bilirubin can lead to pigment stone formation.
High bilirubin levels: Conditions that cause the liver to produce more bilirubin can lead to pigment stone formation.
![]() Concentrated bile: If the gallbladder doesn't empty completely or frequently enough, bile becomes overly concentrated, increasing the risk of stone formation.
Concentrated bile: If the gallbladder doesn't empty completely or frequently enough, bile becomes overly concentrated, increasing the risk of stone formation.
![]() Female sex: Women are more likely to develop gallstones than men, possibly due to the effects of estrogen on cholesterol levels.
Female sex: Women are more likely to develop gallstones than men, possibly due to the effects of estrogen on cholesterol levels.
![]() Pregnancy: Pregnancy increases the risk of gallstones due to hormonal changes and slower gallbladder emptying.
Pregnancy: Pregnancy increases the risk of gallstones due to hormonal changes and slower gallbladder emptying.
![]() Obesity: Excess weight increases cholesterol production and the risk of gallstones.
Obesity: Excess weight increases cholesterol production and the risk of gallstones.
![]() Rapid weight loss: Losing weight quickly can cause the liver to release more cholesterol into the bile.
Rapid weight loss: Losing weight quickly can cause the liver to release more cholesterol into the bile.
![]() Diet: A diet high in fat and cholesterol and low in fiber may increase the risk.
Diet: A diet high in fat and cholesterol and low in fiber may increase the risk.
![]() Age: The risk of gallstones increases with age.
Age: The risk of gallstones increases with age.
![]() Family history: Having a family history of gallstones makes you more likely to develop them.
Family history: Having a family history of gallstones makes you more likely to develop them.
![]() Certain medical conditions: Diabetes, Crohn's disease, ulcerative colitis, sickle cell anemia, and liver cirrhosis can increase the risk.
Certain medical conditions: Diabetes, Crohn's disease, ulcerative colitis, sickle cell anemia, and liver cirrhosis can increase the risk.
![]() Certain medications: Some medications, such as certain cholesterol-lowering drugs and hormone therapy, can increase the risk.
Certain medications: Some medications, such as certain cholesterol-lowering drugs and hormone therapy, can increase the risk.
![]() Ethnicity: Certain ethnic groups, such as Native Americans and Mexican Americans, have a higher risk of gallstones.
Ethnicity: Certain ethnic groups, such as Native Americans and Mexican Americans, have a higher risk of gallstones.
Symptoms:
Many people with gallstones (estimated 80%) don't experience any symptoms. These are often called "silent gallstones." Symptoms usually appear when a gallstone blocks a bile duct:
![]() Sudden, intense pain in the upper right or center of the abdomen: This pain, often called a "gallbladder attack" or biliary colic, can last from several minutes to a few hours. It often occurs after eating a fatty meal.
Sudden, intense pain in the upper right or center of the abdomen: This pain, often called a "gallbladder attack" or biliary colic, can last from several minutes to a few hours. It often occurs after eating a fatty meal.
![]() Pain that radiates to the back or right shoulder:
Pain that radiates to the back or right shoulder:
![]() Nausea and vomiting:
Nausea and vomiting:
![]() Jaundice (yellowing of the skin and eyes): This occurs if a stone blocks the common bile duct, preventing bilirubin from being excreted.
Jaundice (yellowing of the skin and eyes): This occurs if a stone blocks the common bile duct, preventing bilirubin from being excreted.
![]() Fever and chills: These symptoms may indicate an infection of the gallbladder (cholecystitis) or bile ducts (cholangitis), which is a serious complication.
Fever and chills: These symptoms may indicate an infection of the gallbladder (cholecystitis) or bile ducts (cholangitis), which is a serious complication.
![]() Clay-colored stools: This can occur if bile isn't reaching the intestines.
Clay-colored stools: This can occur if bile isn't reaching the intestines.
![]() Dark urine: This can occur if bilirubin is being excreted in the urine.
Dark urine: This can occur if bilirubin is being excreted in the urine.
Diagnosis:
![]() Physical Exam: The doctor will ask about your symptoms and medical history and perform a physical exam.
Physical Exam: The doctor will ask about your symptoms and medical history and perform a physical exam.
![]() Blood tests: To check for signs of infection, inflammation, or liver problems.
Blood tests: To check for signs of infection, inflammation, or liver problems.
![]() Abdominal ultrasound: This is the most common imaging test used to diagnose gallstones. It's non-invasive and can clearly visualize the gallbladder and any stones present.
Abdominal ultrasound: This is the most common imaging test used to diagnose gallstones. It's non-invasive and can clearly visualize the gallbladder and any stones present.
![]() CT scan (Computed Tomography): May be used if ultrasound isn't clear or to rule out other conditions.
CT scan (Computed Tomography): May be used if ultrasound isn't clear or to rule out other conditions.
![]() MRCP (Magnetic Resonance Cholangiopancreatography): A special type of MRI that provides detailed images of the bile ducts and pancreas. It's often used to look for stones in the bile ducts.
MRCP (Magnetic Resonance Cholangiopancreatography): A special type of MRI that provides detailed images of the bile ducts and pancreas. It's often used to look for stones in the bile ducts.
![]() Endoscopic Ultrasound (EUS): An ultrasound probe is attached to an endoscope (a long, flexible tube) that is inserted through the mouth and into the stomach and small intestine. This provides very detailed images of the gallbladder and bile ducts.
Endoscopic Ultrasound (EUS): An ultrasound probe is attached to an endoscope (a long, flexible tube) that is inserted through the mouth and into the stomach and small intestine. This provides very detailed images of the gallbladder and bile ducts.
![]() HIDA scan (Hepatobiliary Iminodiacetic Acid scan): This nuclear medicine test measures how well the gallbladder is functioning.
HIDA scan (Hepatobiliary Iminodiacetic Acid scan): This nuclear medicine test measures how well the gallbladder is functioning.
Treatment:
Treatment depends on whether you have symptoms and the severity of your condition.
![]() Asymptomatic Gallstones (Silent Gallstones): If you have no symptoms, treatment is usually not necessary. The doctor may recommend a "watchful waiting" approach. You should be aware of the symptoms of gallstones and seek medical attention if they develop.
Asymptomatic Gallstones (Silent Gallstones): If you have no symptoms, treatment is usually not necessary. The doctor may recommend a "watchful waiting" approach. You should be aware of the symptoms of gallstones and seek medical attention if they develop.
![]() Symptomatic Gallstones:
Symptomatic Gallstones:![]()

![]() Cholecystectomy (Gallbladder Removal): This is the most common treatment for gallstones. It can be performed in two ways:
Cholecystectomy (Gallbladder Removal): This is the most common treatment for gallstones. It can be performed in two ways:![]()

![]() Laparoscopic Cholecystectomy: This is the preferred method. It involves making several small incisions in the abdomen and using a camera and specialized instruments to remove the gallbladder. It's less invasive, results in less pain and scarring, and has a shorter recovery time.
Laparoscopic Cholecystectomy: This is the preferred method. It involves making several small incisions in the abdomen and using a camera and specialized instruments to remove the gallbladder. It's less invasive, results in less pain and scarring, and has a shorter recovery time.![]()

![]() Open Cholecystectomy: This involves making a larger incision in the abdomen to remove the gallbladder. It's typically used in more complex cases, such as when the gallbladder is severely inflamed or there are complications during a laparoscopic procedure.
Open Cholecystectomy: This involves making a larger incision in the abdomen to remove the gallbladder. It's typically used in more complex cases, such as when the gallbladder is severely inflamed or there are complications during a laparoscopic procedure.![]()

![]() Medications (Ursodiol): This medication can dissolve cholesterol gallstones. However, it takes months or years to work, and the stones may return after treatment is stopped. It's typically used for small cholesterol stones and in people who aren't good candidates for surgery.
Medications (Ursodiol): This medication can dissolve cholesterol gallstones. However, it takes months or years to work, and the stones may return after treatment is stopped. It's typically used for small cholesterol stones and in people who aren't good candidates for surgery.![]()

![]() ERCP (Endoscopic Retrograde Cholangiopancreatography): This procedure is used to remove stones that have moved into the bile ducts. An endoscope is inserted through the mouth and into the small intestine. A catheter is then inserted into the bile duct to retrieve the stones. This is usually done before or after a cholecystectomy.
ERCP (Endoscopic Retrograde Cholangiopancreatography): This procedure is used to remove stones that have moved into the bile ducts. An endoscope is inserted through the mouth and into the small intestine. A catheter is then inserted into the bile duct to retrieve the stones. This is usually done before or after a cholecystectomy.
Complications:
If left untreated, gallstones can lead to serious complications:
![]() Cholecystitis (Inflammation of the gallbladder): This can cause severe pain, fever, and infection.
Cholecystitis (Inflammation of the gallbladder): This can cause severe pain, fever, and infection.
![]() Choledocholithiasis (Stones in the bile ducts): This can block the flow of bile and cause jaundice, infection, and pancreatitis.
Choledocholithiasis (Stones in the bile ducts): This can block the flow of bile and cause jaundice, infection, and pancreatitis.
![]() Cholangitis (Infection of the bile ducts): This is a serious infection that can be life-threatening.
Cholangitis (Infection of the bile ducts): This is a serious infection that can be life-threatening.
![]() Pancreatitis (Inflammation of the pancreas): Gallstones can block the pancreatic duct, leading to pancreatitis.
Pancreatitis (Inflammation of the pancreas): Gallstones can block the pancreatic duct, leading to pancreatitis.
![]() Gallbladder cancer: While rare, chronic inflammation caused by gallstones can increase the risk of gallbladder cancer.
Gallbladder cancer: While rare, chronic inflammation caused by gallstones can increase the risk of gallbladder cancer.
Prevention:
While you can't completely eliminate the risk of gallstones, you can take steps to reduce your chances:
![]() Maintain a healthy weight: Avoid obesity and rapid weight loss.
Maintain a healthy weight: Avoid obesity and rapid weight loss.
![]() Eat a healthy diet: Consume a diet low in fat and cholesterol and high in fiber.
Eat a healthy diet: Consume a diet low in fat and cholesterol and high in fiber.
![]() Exercise regularly:
Exercise regularly:
![]() Consider medications (if at high risk): If you have a high risk of gallstones (e.g., after bariatric surgery), your doctor may recommend ursodiol to help prevent them.
Consider medications (if at high risk): If you have a high risk of gallstones (e.g., after bariatric surgery), your doctor may recommend ursodiol to help prevent them.
![]() Avoid skipping meals: This can help prevent bile from becoming overly concentrated.
Avoid skipping meals: This can help prevent bile from becoming overly concentrated.
In summary, gallstones are common, and while many people don't experience any symptoms, they can cause significant pain and complications if they block the bile ducts. If you suspect you have gallstones, it's important to see a doctor for diagnosis and treatment.