Genital arterial disease Atherosclerosis (Arteriosclerosis)
Published: 18 Jun 2025
ICD9: 443.9 ICD10: I73.9 ICD11: BD40
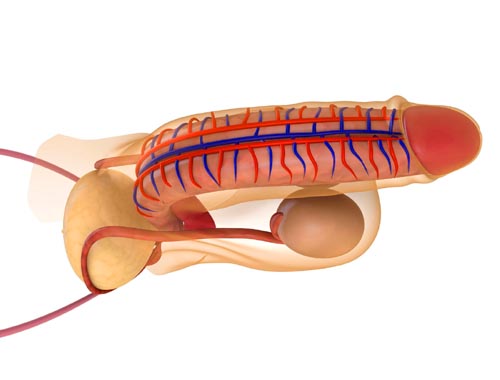
Genital arterial disease due to atherosclerosis (or arteriosclerosis) refers to the narrowing and hardening of the arteries that supply blood to the penis and surrounding genital tissues due to plaque buildup.
Let's break that down:
![]() Atherosclerosis/Arteriosclerosis: These terms are often used interchangeably, although technically they're slightly different. Atherosclerosis is a *type* of arteriosclerosis. It's characterized by the accumulation of fatty deposits, cholesterol, cellular waste products, calcium, and other substances (collectively called plaque) along the inner walls of arteries. This plaque build-up leads to the arteries becoming narrowed, hardened, and less flexible.
Atherosclerosis/Arteriosclerosis: These terms are often used interchangeably, although technically they're slightly different. Atherosclerosis is a *type* of arteriosclerosis. It's characterized by the accumulation of fatty deposits, cholesterol, cellular waste products, calcium, and other substances (collectively called plaque) along the inner walls of arteries. This plaque build-up leads to the arteries becoming narrowed, hardened, and less flexible.
![]() Genital Arteries: These are the arteries that are responsible for bringing blood to the penis and the tissues around the genitals (like the scrotum). Proper blood flow is essential for normal sexual function, particularly erections.
Genital Arteries: These are the arteries that are responsible for bringing blood to the penis and the tissues around the genitals (like the scrotum). Proper blood flow is essential for normal sexual function, particularly erections.
![]() Disease/Condition: The presence of atherosclerotic plaque in these arteries significantly impairs blood flow. Reduced blood flow can lead to various symptoms and complications.
Disease/Condition: The presence of atherosclerotic plaque in these arteries significantly impairs blood flow. Reduced blood flow can lead to various symptoms and complications.
What are the consequences/symptoms?
The most significant consequence of genital arterial disease due to atherosclerosis is erectile dysfunction (ED). Since an erection relies on adequate blood flow to the penis, narrowed arteries make it difficult or impossible to achieve and maintain an erection firm enough for satisfactory sexual intercourse.
Other possible symptoms, though often less pronounced:
![]() Reduced libido (sex drive): Reduced blood flow can affect hormonal balance and nerve function, contributing to lower sex drive.
Reduced libido (sex drive): Reduced blood flow can affect hormonal balance and nerve function, contributing to lower sex drive.
![]() Pain or discomfort in the genital area: While less common, severely restricted blood flow can, in rare cases, cause pain.
Pain or discomfort in the genital area: While less common, severely restricted blood flow can, in rare cases, cause pain.
![]() Changes in the appearance or sensation of the penis: In chronic cases, decreased blood flow could theoretically contribute to tissue changes, but this is less prominent.
Changes in the appearance or sensation of the penis: In chronic cases, decreased blood flow could theoretically contribute to tissue changes, but this is less prominent.
Risk Factors:
The risk factors for atherosclerosis in the genital arteries are the same as those for atherosclerosis elsewhere in the body:
![]() Age: Risk increases with age.
Age: Risk increases with age.
![]() High cholesterol: Elevated LDL ("bad") cholesterol contributes to plaque formation.
High cholesterol: Elevated LDL ("bad") cholesterol contributes to plaque formation.
![]() High blood pressure (Hypertension): Damages artery walls, making them more prone to plaque accumulation.
High blood pressure (Hypertension): Damages artery walls, making them more prone to plaque accumulation.
![]() Smoking: Damages blood vessels and promotes plaque formation.
Smoking: Damages blood vessels and promotes plaque formation.
![]() Diabetes: High blood sugar levels damage artery walls.
Diabetes: High blood sugar levels damage artery walls.
![]() Obesity: Associated with other risk factors like high cholesterol, high blood pressure, and diabetes.
Obesity: Associated with other risk factors like high cholesterol, high blood pressure, and diabetes.
![]() Family history of heart disease: Genetic predisposition increases the risk.
Family history of heart disease: Genetic predisposition increases the risk.
![]() Lack of physical activity: Contributes to obesity and other risk factors.
Lack of physical activity: Contributes to obesity and other risk factors.
![]() Unhealthy diet: A diet high in saturated and trans fats, cholesterol, and sodium increases the risk of atherosclerosis.
Unhealthy diet: A diet high in saturated and trans fats, cholesterol, and sodium increases the risk of atherosclerosis.
Diagnosis:
Diagnosis typically involves:
![]() Medical history and physical examination: A doctor will ask about your symptoms, risk factors, and medical history.
Medical history and physical examination: A doctor will ask about your symptoms, risk factors, and medical history.
![]() Doppler ultrasound: This non-invasive test uses sound waves to measure blood flow in the penile arteries. It can help identify areas of narrowing or blockage.
Doppler ultrasound: This non-invasive test uses sound waves to measure blood flow in the penile arteries. It can help identify areas of narrowing or blockage.
![]() Angiography: A more invasive test where a dye is injected into the arteries, and X-rays are taken to visualize the blood vessels. This is usually reserved for cases where other tests are inconclusive or if surgery is being considered.
Angiography: A more invasive test where a dye is injected into the arteries, and X-rays are taken to visualize the blood vessels. This is usually reserved for cases where other tests are inconclusive or if surgery is being considered.
![]() Blood tests: To check cholesterol levels, blood sugar, and other indicators of cardiovascular health.
Blood tests: To check cholesterol levels, blood sugar, and other indicators of cardiovascular health.
Treatment:
Treatment aims to:
1. Manage underlying risk factors:![]()

![]() Lifestyle changes (diet, exercise, smoking cessation)
Lifestyle changes (diet, exercise, smoking cessation)![]()

![]() Medications to lower cholesterol, control blood pressure, and manage diabetes.
Medications to lower cholesterol, control blood pressure, and manage diabetes.
2. Improve blood flow:![]()

![]() Medications for Erectile Dysfunction: PDE5 inhibitors (e.g., sildenafil, tadalafil) are commonly prescribed to help improve blood flow to the penis. They don't treat the underlying atherosclerosis, but they can help manage the symptoms.
Medications for Erectile Dysfunction: PDE5 inhibitors (e.g., sildenafil, tadalafil) are commonly prescribed to help improve blood flow to the penis. They don't treat the underlying atherosclerosis, but they can help manage the symptoms.![]()

![]() Injections: Injecting medication directly into the penis to promote blood flow.
Injections: Injecting medication directly into the penis to promote blood flow.![]()

![]() Vacuum devices: Devices that create a vacuum to draw blood into the penis.
Vacuum devices: Devices that create a vacuum to draw blood into the penis.![]()

![]() Surgery: In rare cases, surgery to bypass blocked arteries or implant a penile prosthesis may be considered. However, surgery is usually a last resort.
Surgery: In rare cases, surgery to bypass blocked arteries or implant a penile prosthesis may be considered. However, surgery is usually a last resort.
Important Considerations:
![]() Erectile dysfunction can be an early warning sign of cardiovascular disease. Because the penile arteries are smaller than other arteries in the body, they can be affected by atherosclerosis earlier than larger arteries. Therefore, ED can be a sign that you may have or are at risk for heart disease, stroke, or other vascular problems.
Erectile dysfunction can be an early warning sign of cardiovascular disease. Because the penile arteries are smaller than other arteries in the body, they can be affected by atherosclerosis earlier than larger arteries. Therefore, ED can be a sign that you may have or are at risk for heart disease, stroke, or other vascular problems.
![]() Consult a doctor: If you are experiencing symptoms of erectile dysfunction, it's essential to see a doctor to get a diagnosis and discuss treatment options. Don't self-diagnose or self-treat.
Consult a doctor: If you are experiencing symptoms of erectile dysfunction, it's essential to see a doctor to get a diagnosis and discuss treatment options. Don't self-diagnose or self-treat.
![]() Lifestyle changes are crucial: Regardless of other treatments, lifestyle changes are essential for managing the underlying cause of the problem and preventing further progression of atherosclerosis.
Lifestyle changes are crucial: Regardless of other treatments, lifestyle changes are essential for managing the underlying cause of the problem and preventing further progression of atherosclerosis.
In summary, genital arterial disease due to atherosclerosis is a condition where plaque buildup in the arteries supplying the penis and genitals reduces blood flow, leading to erectile dysfunction and potentially other problems. It is linked to the same risk factors as heart disease and requires medical evaluation and treatment.