Giant Cell Arteritis (Temporal arteritis, Cranial arteritis)
Published: 18 Jun 2025
ICD9: 446.5 ICD10: M31.6 ICD11: 4A44.2
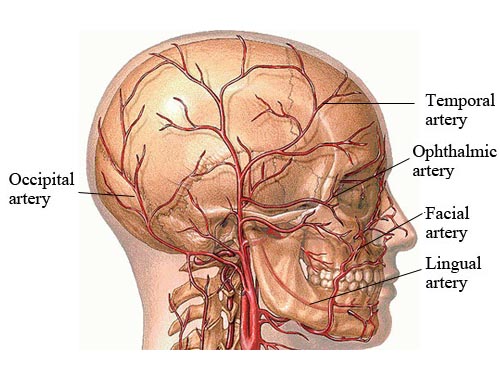
Giant cell arteritis (GCA), also known as temporal arteritis or cranial arteritis, is an inflammatory condition affecting medium-sized and large arteries, most commonly the arteries of the head, especially the temporal arteries.
It's a serious condition that can lead to blindness and other complications if left untreated.
Here's a breakdown of the key aspects:
What it is:
![]() Inflammation of Arteries: GCA is characterized by inflammation of the walls of arteries. This inflammation causes the artery to narrow, reducing blood flow.
Inflammation of Arteries: GCA is characterized by inflammation of the walls of arteries. This inflammation causes the artery to narrow, reducing blood flow.
![]() Giant Cells: The name "giant cell arteritis" comes from the presence of large, abnormal cells (giant cells) that are often found in the inflamed artery walls when a biopsy is performed. However, these cells aren't always present.
Giant Cells: The name "giant cell arteritis" comes from the presence of large, abnormal cells (giant cells) that are often found in the inflamed artery walls when a biopsy is performed. However, these cells aren't always present.
![]() Systemic Disease: While often focused on the head and temporal arteries, GCA is a systemic disease, meaning it can affect arteries in other parts of the body, including the aorta (the largest artery in the body) and its major branches. This is then referred to as large vessel arteritis.
Systemic Disease: While often focused on the head and temporal arteries, GCA is a systemic disease, meaning it can affect arteries in other parts of the body, including the aorta (the largest artery in the body) and its major branches. This is then referred to as large vessel arteritis.
Who gets it:
![]() Older Adults: GCA almost exclusively affects older adults, typically over the age of 50. It's most common in people over 70.
Older Adults: GCA almost exclusively affects older adults, typically over the age of 50. It's most common in people over 70.
![]() More Common in Women: Women are more likely to develop GCA than men.
More Common in Women: Women are more likely to develop GCA than men.
![]() More Common in Caucasians: The condition is more frequently seen in people of Northern European descent.
More Common in Caucasians: The condition is more frequently seen in people of Northern European descent.
Symptoms:
Symptoms can vary, but some of the most common include:
![]() New Headache: A persistent, often severe headache, frequently located in the temples. It may be throbbing or constant.
New Headache: A persistent, often severe headache, frequently located in the temples. It may be throbbing or constant.
![]() Temporal Artery Tenderness: Pain or tenderness to the touch over the temporal arteries (the arteries that run along the sides of the head). The artery may feel thickened or cord-like.
Temporal Artery Tenderness: Pain or tenderness to the touch over the temporal arteries (the arteries that run along the sides of the head). The artery may feel thickened or cord-like.
![]() Jaw Claudication: Pain or fatigue in the jaw muscles while chewing. This is a classic symptom.
Jaw Claudication: Pain or fatigue in the jaw muscles while chewing. This is a classic symptom.
![]() Visual Disturbances: Blurred vision, double vision, temporary vision loss (amaurosis fugax), or even permanent vision loss. This is a *medical emergency* requiring immediate treatment.
Visual Disturbances: Blurred vision, double vision, temporary vision loss (amaurosis fugax), or even permanent vision loss. This is a *medical emergency* requiring immediate treatment.
![]() Scalp Tenderness: Pain or sensitivity on the scalp.
Scalp Tenderness: Pain or sensitivity on the scalp.
![]() Fever: Low-grade fever.
Fever: Low-grade fever.
![]() Fatigue: Feeling unusually tired and weak.
Fatigue: Feeling unusually tired and weak.
![]() Muscle Aches and Stiffness: Often associated with Polymyalgia Rheumatica (PMR), which frequently occurs alongside GCA. PMR causes pain and stiffness in the neck, shoulders, and hips.
Muscle Aches and Stiffness: Often associated with Polymyalgia Rheumatica (PMR), which frequently occurs alongside GCA. PMR causes pain and stiffness in the neck, shoulders, and hips.
![]() Weight Loss: Unexplained weight loss.
Weight Loss: Unexplained weight loss.
Diagnosis:
![]() Physical Exam and Medical History: The doctor will ask about your symptoms and perform a physical exam, paying close attention to the temporal arteries.
Physical Exam and Medical History: The doctor will ask about your symptoms and perform a physical exam, paying close attention to the temporal arteries.
![]() Blood Tests:
Blood Tests:![]()

![]() Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These are blood tests that measure inflammation in the body. Elevated levels strongly suggest GCA. However, normal levels do *not* rule it out.
Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These are blood tests that measure inflammation in the body. Elevated levels strongly suggest GCA. However, normal levels do *not* rule it out.![]()

![]() Complete Blood Count (CBC): This can show elevated white blood cell counts, indicating inflammation.
Complete Blood Count (CBC): This can show elevated white blood cell counts, indicating inflammation.
![]() Temporal Artery Biopsy: This is the *gold standard* for diagnosis. A small sample of the temporal artery is removed and examined under a microscope for signs of inflammation and giant cells. A negative biopsy doesn't always rule out GCA because the inflammation can be patchy.
Temporal Artery Biopsy: This is the *gold standard* for diagnosis. A small sample of the temporal artery is removed and examined under a microscope for signs of inflammation and giant cells. A negative biopsy doesn't always rule out GCA because the inflammation can be patchy.
![]() Imaging Studies: In some cases, imaging techniques like ultrasound, MRI, or PET scans may be used to visualize the arteries and look for signs of inflammation. Duplex ultrasound is a helpful non-invasive method for assessing cranial arteries.
Imaging Studies: In some cases, imaging techniques like ultrasound, MRI, or PET scans may be used to visualize the arteries and look for signs of inflammation. Duplex ultrasound is a helpful non-invasive method for assessing cranial arteries.
Treatment:
![]() Corticosteroids (Prednisone): The primary treatment for GCA is high-dose corticosteroids, such as prednisone. These medications quickly reduce inflammation and prevent further damage, especially vision loss. Treatment is usually started immediately if GCA is suspected, even before a biopsy is performed, due to the risk of blindness.
Corticosteroids (Prednisone): The primary treatment for GCA is high-dose corticosteroids, such as prednisone. These medications quickly reduce inflammation and prevent further damage, especially vision loss. Treatment is usually started immediately if GCA is suspected, even before a biopsy is performed, due to the risk of blindness.
![]() Low-Dose Aspirin: Aspirin is sometimes prescribed to help prevent blood clots and reduce the risk of stroke.
Low-Dose Aspirin: Aspirin is sometimes prescribed to help prevent blood clots and reduce the risk of stroke.
![]() Tocilizumab (Actemra): This is a biologic medication that targets a specific inflammatory protein (IL-6). It can be used as an alternative or in addition to corticosteroids, especially to help reduce the steroid dose or prevent relapses.
Tocilizumab (Actemra): This is a biologic medication that targets a specific inflammatory protein (IL-6). It can be used as an alternative or in addition to corticosteroids, especially to help reduce the steroid dose or prevent relapses.
![]() Tapering: After the initial treatment period, the corticosteroid dose is gradually tapered down over many months or even years to minimize side effects.
Tapering: After the initial treatment period, the corticosteroid dose is gradually tapered down over many months or even years to minimize side effects.
![]() Monitoring: Regular follow-up appointments and blood tests are essential to monitor the disease activity, adjust medications, and watch for any complications or side effects.
Monitoring: Regular follow-up appointments and blood tests are essential to monitor the disease activity, adjust medications, and watch for any complications or side effects.
Complications:
![]() Blindness: The most feared complication is irreversible vision loss due to inflammation affecting the arteries that supply the optic nerve. Prompt treatment is crucial to prevent this.
Blindness: The most feared complication is irreversible vision loss due to inflammation affecting the arteries that supply the optic nerve. Prompt treatment is crucial to prevent this.
![]() Stroke: Inflammation can damage arteries in the brain, increasing the risk of stroke.
Stroke: Inflammation can damage arteries in the brain, increasing the risk of stroke.
![]() Aortic Aneurysm or Dissection: GCA can affect the aorta, leading to a weakened and enlarged section (aneurysm) or a tear in the aortic wall (dissection). These are serious and potentially life-threatening.
Aortic Aneurysm or Dissection: GCA can affect the aorta, leading to a weakened and enlarged section (aneurysm) or a tear in the aortic wall (dissection). These are serious and potentially life-threatening.
![]() Polymyalgia Rheumatica (PMR): As mentioned earlier, GCA is often associated with PMR.
Polymyalgia Rheumatica (PMR): As mentioned earlier, GCA is often associated with PMR.
In summary, Giant Cell Arteritis is a serious inflammatory condition that requires prompt diagnosis and treatment to prevent potentially devastating complications, particularly vision loss. If you experience symptoms suggestive of GCA, it's essential to seek medical attention immediately.