Glioblastoma (brain tumor)
Published: 18 Jun 2025
ICD9: 191.9 ICD10: C71.9 ICD11: 2A00.00
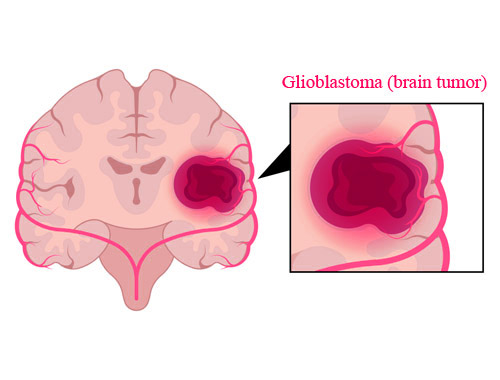
Glioblastoma (GBM) is the most aggressive type of cancer that starts in the brain.
It's classified as a grade IV astrocytoma, meaning it arises from astrocytes, a type of glial cell that supports nerve cells in the brain.
Here's a breakdown of key aspects:
What it is:
![]() Type of Tumor: It's a malignant (cancerous) tumor.
Type of Tumor: It's a malignant (cancerous) tumor.
![]() Location: Typically occurs in the cerebral hemispheres (the largest part of the brain), but can occur anywhere in the brain or spinal cord.
Location: Typically occurs in the cerebral hemispheres (the largest part of the brain), but can occur anywhere in the brain or spinal cord.
![]() Origin: Arises from astrocytes, which are star-shaped glial cells that provide support and nourishment to neurons.
Origin: Arises from astrocytes, which are star-shaped glial cells that provide support and nourishment to neurons.
![]() Grade: Classified as a Grade IV astrocytoma, indicating its high degree of malignancy and rapid growth.
Grade: Classified as a Grade IV astrocytoma, indicating its high degree of malignancy and rapid growth.
Characteristics:
![]() Aggressive Growth: GBMs grow rapidly and aggressively, invading surrounding brain tissue.
Aggressive Growth: GBMs grow rapidly and aggressively, invading surrounding brain tissue.
![]() Poorly Defined Borders: Unlike some other tumors, GBMs often have irregular shapes and indistinct borders, making complete surgical removal difficult.
Poorly Defined Borders: Unlike some other tumors, GBMs often have irregular shapes and indistinct borders, making complete surgical removal difficult.
![]() Vascularity: These tumors often have abnormal blood vessels that leak, causing swelling (edema) in the brain.
Vascularity: These tumors often have abnormal blood vessels that leak, causing swelling (edema) in the brain.
![]() Necrosis: Areas of dead tissue (necrosis) are common within GBMs.
Necrosis: Areas of dead tissue (necrosis) are common within GBMs.
![]() Heterogeneity: GBMs are highly heterogeneous, meaning that different cells within the tumor can have different genetic and molecular characteristics. This makes treatment challenging.
Heterogeneity: GBMs are highly heterogeneous, meaning that different cells within the tumor can have different genetic and molecular characteristics. This makes treatment challenging.
Symptoms:
Symptoms vary depending on the tumor's size, location, and rate of growth. Common symptoms include:
![]() Headaches: Often persistent and may be worse in the morning.
Headaches: Often persistent and may be worse in the morning.
![]() Seizures: Can be the first sign of a GBM.
Seizures: Can be the first sign of a GBM.
![]() Nausea and Vomiting: Due to increased pressure within the skull.
Nausea and Vomiting: Due to increased pressure within the skull.
![]() Weakness or Numbness: Affecting one side of the body.
Weakness or Numbness: Affecting one side of the body.
![]() Speech Difficulties: Trouble finding words or understanding language.
Speech Difficulties: Trouble finding words or understanding language.
![]() Vision Problems: Blurred vision, double vision, or loss of peripheral vision.
Vision Problems: Blurred vision, double vision, or loss of peripheral vision.
![]() Personality Changes: Irritability, confusion, or changes in behavior.
Personality Changes: Irritability, confusion, or changes in behavior.
![]() Memory Problems: Difficulty with short-term or long-term memory.
Memory Problems: Difficulty with short-term or long-term memory.
Causes:
The exact cause of GBM is not fully understood. Most cases are *de novo*, meaning they arise spontaneously without a known genetic predisposition. Risk factors are rare and not well-defined, but may include:
![]() Age: GBMs are more common in older adults (typically 45-70 years old).
Age: GBMs are more common in older adults (typically 45-70 years old).
![]() Radiation Exposure: Prior exposure to ionizing radiation to the head.
Radiation Exposure: Prior exposure to ionizing radiation to the head.
![]() Genetic Syndromes: Rare genetic conditions, such as neurofibromatosis type 1, tuberous sclerosis, and Li-Fraumeni syndrome, can increase the risk.
Genetic Syndromes: Rare genetic conditions, such as neurofibromatosis type 1, tuberous sclerosis, and Li-Fraumeni syndrome, can increase the risk.
![]() Sex: Slightly more common in males.
Sex: Slightly more common in males.
Diagnosis:
Diagnosis typically involves:
![]() Neurological Examination: To assess neurological function.
Neurological Examination: To assess neurological function.
![]() MRI (Magnetic Resonance Imaging): Provides detailed images of the brain to detect the tumor.
MRI (Magnetic Resonance Imaging): Provides detailed images of the brain to detect the tumor.
![]() CT Scan (Computed Tomography): Can also be used to visualize the brain.
CT Scan (Computed Tomography): Can also be used to visualize the brain.
![]() Biopsy: A sample of the tumor is taken (usually during surgery) and examined under a microscope to confirm the diagnosis and determine the tumor's characteristics.
Biopsy: A sample of the tumor is taken (usually during surgery) and examined under a microscope to confirm the diagnosis and determine the tumor's characteristics.
![]() Molecular Testing: Tests performed on the tumor tissue to identify specific genetic mutations or other molecular markers that can help guide treatment decisions.
Molecular Testing: Tests performed on the tumor tissue to identify specific genetic mutations or other molecular markers that can help guide treatment decisions.
Treatment:
Treatment is complex and often involves a combination of approaches:
![]() Surgery: To remove as much of the tumor as possible without causing significant neurological damage. Complete resection is often impossible due to the infiltrative nature of the tumor.
Surgery: To remove as much of the tumor as possible without causing significant neurological damage. Complete resection is often impossible due to the infiltrative nature of the tumor.
![]() Radiation Therapy: To kill remaining cancer cells after surgery.
Radiation Therapy: To kill remaining cancer cells after surgery.
![]() Chemotherapy: Typically Temozolomide (TMZ), an oral chemotherapy drug, is used. It is often given concurrently with radiation therapy and then as maintenance therapy.
Chemotherapy: Typically Temozolomide (TMZ), an oral chemotherapy drug, is used. It is often given concurrently with radiation therapy and then as maintenance therapy.
![]() Tumor Treating Fields (TTFields): Uses electric fields to disrupt cancer cell division.
Tumor Treating Fields (TTFields): Uses electric fields to disrupt cancer cell division.
![]() Targeted Therapy: Drugs that target specific molecules or pathways involved in tumor growth (e.g., bevacizumab, which targets blood vessel formation).
Targeted Therapy: Drugs that target specific molecules or pathways involved in tumor growth (e.g., bevacizumab, which targets blood vessel formation).
![]() Clinical Trials: Participation in clinical trials may offer access to new and experimental therapies.
Clinical Trials: Participation in clinical trials may offer access to new and experimental therapies.
![]() Supportive Care: To manage symptoms and improve quality of life. This can include steroids to reduce swelling, anti-seizure medications, and rehabilitation therapies.
Supportive Care: To manage symptoms and improve quality of life. This can include steroids to reduce swelling, anti-seizure medications, and rehabilitation therapies.
Prognosis:
The prognosis for GBM is generally poor. The median survival time is typically around 12-18 months with standard treatment. However, survival rates can vary depending on factors such as:
![]() Age: Younger patients tend to have a better prognosis.
Age: Younger patients tend to have a better prognosis.
![]() Extent of Surgical Resection: Removing more of the tumor is associated with longer survival.
Extent of Surgical Resection: Removing more of the tumor is associated with longer survival.
![]() Performance Status: A patient's overall health and functional ability.
Performance Status: A patient's overall health and functional ability.
![]() Molecular Markers: Certain genetic mutations (e.g., MGMT promoter methylation) are associated with a better response to chemotherapy. IDH mutation is generally associated with better outcomes, but is uncommon in GBM.
Molecular Markers: Certain genetic mutations (e.g., MGMT promoter methylation) are associated with a better response to chemotherapy. IDH mutation is generally associated with better outcomes, but is uncommon in GBM.
Important Considerations:
![]() Individualized Treatment: Treatment plans are tailored to each patient's specific situation.
Individualized Treatment: Treatment plans are tailored to each patient's specific situation.
![]() Second Opinions: Seeking a second opinion from a neuro-oncologist is often recommended.
Second Opinions: Seeking a second opinion from a neuro-oncologist is often recommended.
![]() Palliative Care: Focuses on managing symptoms and improving quality of life for patients with advanced GBM.
Palliative Care: Focuses on managing symptoms and improving quality of life for patients with advanced GBM.
![]() Research: Ongoing research is aimed at developing new and more effective treatments for GBM.
Research: Ongoing research is aimed at developing new and more effective treatments for GBM.
This information is for general knowledge and should not be considered medical advice. If you have concerns about your health, please consult with a qualified healthcare professional.