Hepatic encephalopathy
Published: 18 Jun 2025
ICD9: 572.2 ICD10: K76.82 ICD11: DB99.5
Hepatic encephalopathy (HE) is a decline in brain function that occurs as a result of severe liver disease.
Essentially, it's when toxins that the liver normally filters out of the blood build up in the bloodstream and affect the brain.
Here's a breakdown:
![]() Hepatic: Refers to the liver.
Hepatic: Refers to the liver.
![]() Encephalopathy: A general term meaning disease or damage of the brain.
Encephalopathy: A general term meaning disease or damage of the brain.
How it happens:
The liver plays a crucial role in detoxifying the blood, removing harmful substances produced by the body's metabolism. When the liver is severely damaged, it can't perform this function effectively. As a result, toxins like ammonia, which are normally converted into less harmful substances (like urea to be excreted by the kidneys), accumulate in the blood. These toxins then travel to the brain, where they can interfere with brain function.
Causes:
HE typically occurs in people with chronic liver disease, such as:
![]() Cirrhosis: Scarring of the liver, often caused by alcohol abuse, viral hepatitis (B or C), or non-alcoholic fatty liver disease (NAFLD).
Cirrhosis: Scarring of the liver, often caused by alcohol abuse, viral hepatitis (B or C), or non-alcoholic fatty liver disease (NAFLD).
![]() Acute liver failure: Sudden and severe liver damage from infections, drugs, or toxins.
Acute liver failure: Sudden and severe liver damage from infections, drugs, or toxins.
![]() Shunts: Abnormal blood vessels that bypass the liver, allowing toxins to enter the bloodstream directly.
Shunts: Abnormal blood vessels that bypass the liver, allowing toxins to enter the bloodstream directly.
Symptoms:
The symptoms of HE can vary widely depending on the severity of the condition and can fluctuate. They can range from subtle changes in mental function to coma. Common symptoms include:
![]() Mild:
Mild:![]()

![]() Changes in sleep patterns (e.g., sleeping during the day, being awake at night)
Changes in sleep patterns (e.g., sleeping during the day, being awake at night)![]()

![]() Mild confusion
Mild confusion![]()

![]() Forgetfulness
Forgetfulness![]()

![]() Irritability
Irritability![]()

![]() Personality changes
Personality changes![]()

![]() Difficulty concentrating
Difficulty concentrating![]()

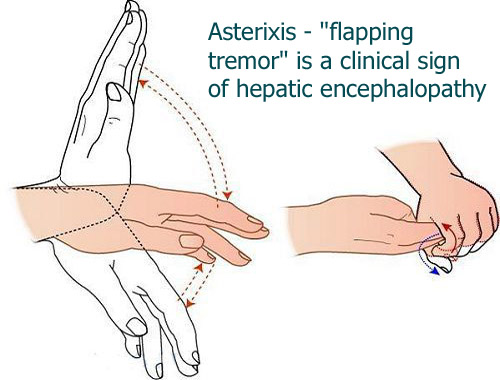
![]() Hand tremor (asterixis, a flapping tremor of the hands when the wrist is extended)
Hand tremor (asterixis, a flapping tremor of the hands when the wrist is extended)![]()

![]() Slurred speech
Slurred speech
![]() Moderate:
Moderate:![]()

![]() Increased confusion
Increased confusion![]()

![]() Disorientation (not knowing time, place, or person)
Disorientation (not knowing time, place, or person)![]()

![]() Lethargy
Lethargy![]()

![]() Marked asterixis
Marked asterixis
![]() Severe:
Severe:![]()

![]() Severe confusion
Severe confusion![]()

![]() Stupor (reduced level of consciousness)
Stupor (reduced level of consciousness)![]()

![]() Coma
Coma
Diagnosis:
Diagnosis usually involves:
![]() Physical exam: To assess mental status and look for signs of liver disease.
Physical exam: To assess mental status and look for signs of liver disease.
![]() Blood tests: To check liver function, ammonia levels, and rule out other conditions.
Blood tests: To check liver function, ammonia levels, and rule out other conditions.
![]() Electroencephalogram (EEG): To measure brain activity.
Electroencephalogram (EEG): To measure brain activity.
![]() Imaging tests: Like CT scans or MRIs, to evaluate the liver and rule out other causes of neurological symptoms.
Imaging tests: Like CT scans or MRIs, to evaluate the liver and rule out other causes of neurological symptoms.
![]() Mental status testing: Simple tests to evaluate cognitive function and orientation.
Mental status testing: Simple tests to evaluate cognitive function and orientation.
Treatment:
The goals of treatment are to reduce the levels of toxins in the blood, improve brain function, and manage the underlying liver disease. Treatment options may include:
![]() Lactulose: A sugar that helps to reduce ammonia levels in the body by promoting bowel movements and reducing ammonia absorption in the intestines.
Lactulose: A sugar that helps to reduce ammonia levels in the body by promoting bowel movements and reducing ammonia absorption in the intestines.
![]() Rifaximin: An antibiotic that reduces the number of ammonia-producing bacteria in the gut.
Rifaximin: An antibiotic that reduces the number of ammonia-producing bacteria in the gut.
![]() Dietary changes: Reducing protein intake may be recommended in some cases. However, completely restricting protein is usually not advised, as it can lead to malnutrition. Consulting with a dietician is important.
Dietary changes: Reducing protein intake may be recommended in some cases. However, completely restricting protein is usually not advised, as it can lead to malnutrition. Consulting with a dietician is important.
![]() Treating underlying liver disease: Addressing the underlying cause of the liver damage is crucial for long-term management. This might include antiviral medications for hepatitis, alcohol abstinence, or weight loss for NAFLD.
Treating underlying liver disease: Addressing the underlying cause of the liver damage is crucial for long-term management. This might include antiviral medications for hepatitis, alcohol abstinence, or weight loss for NAFLD.
![]() Liver transplant: In severe cases, a liver transplant may be the only option for survival.
Liver transplant: In severe cases, a liver transplant may be the only option for survival.
Important Considerations:
![]() HE is a serious condition that can be life-threatening if left untreated.
HE is a serious condition that can be life-threatening if left untreated.
![]() Early diagnosis and treatment are crucial to improve outcomes.
Early diagnosis and treatment are crucial to improve outcomes.
![]() Patients with liver disease should be aware of the symptoms of HE and seek medical attention promptly if they experience any changes in mental function.
Patients with liver disease should be aware of the symptoms of HE and seek medical attention promptly if they experience any changes in mental function.
![]() Treatment needs to be tailored to the individual patient's condition and underlying liver disease.
Treatment needs to be tailored to the individual patient's condition and underlying liver disease.
Disclaimer: This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.