Hepatic necrosis
Published: 18 Jun 2025
ICD9: 570 ICD10: K76.2 ICD11: DB97.Y
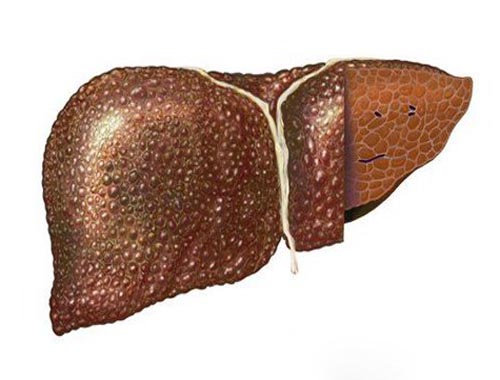
Hepatic necrosis is the death of liver cells (hepatocytes).
It's a serious condition that can lead to liver failure if it's widespread and severe. Think of it as the liver tissue essentially collapsing and dying.
Here's a more detailed breakdown:
![]() Hepatic: Refers to the liver.
Hepatic: Refers to the liver.
![]() Necrosis: Refers to the death of cells or tissues.
Necrosis: Refers to the death of cells or tissues.
Causes of Hepatic Necrosis:
Hepatic necrosis can result from a variety of causes, including:
![]() Drug-induced liver injury (DILI): This is a common cause. Many drugs, both prescription and over-the-counter (especially acetaminophen/paracetamol in high doses), as well as herbal supplements can be toxic to the liver.
Drug-induced liver injury (DILI): This is a common cause. Many drugs, both prescription and over-the-counter (especially acetaminophen/paracetamol in high doses), as well as herbal supplements can be toxic to the liver.
![]() Viral hepatitis: Hepatitis A, B, C, D, and E viruses can cause liver inflammation and necrosis. Acute hepatitis is more likely to cause necrosis than chronic hepatitis.
Viral hepatitis: Hepatitis A, B, C, D, and E viruses can cause liver inflammation and necrosis. Acute hepatitis is more likely to cause necrosis than chronic hepatitis.
![]() Ischemia: Reduced blood flow to the liver (ischemic hepatitis), such as in cases of heart failure, shock, or thrombosis (blood clot), can deprive liver cells of oxygen and nutrients, leading to necrosis.
Ischemia: Reduced blood flow to the liver (ischemic hepatitis), such as in cases of heart failure, shock, or thrombosis (blood clot), can deprive liver cells of oxygen and nutrients, leading to necrosis.
![]() Toxins: Exposure to certain toxins, such as poisonous mushrooms (e.g., *Amanita phalloides*), industrial chemicals (e.g., carbon tetrachloride), or aflatoxins (produced by certain molds), can damage the liver.
Toxins: Exposure to certain toxins, such as poisonous mushrooms (e.g., *Amanita phalloides*), industrial chemicals (e.g., carbon tetrachloride), or aflatoxins (produced by certain molds), can damage the liver.
![]() Alcoholic liver disease: Long-term excessive alcohol consumption can lead to liver inflammation and eventually necrosis (alcoholic hepatitis).
Alcoholic liver disease: Long-term excessive alcohol consumption can lead to liver inflammation and eventually necrosis (alcoholic hepatitis).
![]() Autoimmune hepatitis: The body's immune system attacks liver cells, causing inflammation and necrosis.
Autoimmune hepatitis: The body's immune system attacks liver cells, causing inflammation and necrosis.
![]() Wilson's disease: A genetic disorder that causes copper to accumulate in the liver, leading to damage and necrosis.
Wilson's disease: A genetic disorder that causes copper to accumulate in the liver, leading to damage and necrosis.
![]() Budd-Chiari syndrome: Blockage of the hepatic veins, which drain blood from the liver, leading to congestion and necrosis.
Budd-Chiari syndrome: Blockage of the hepatic veins, which drain blood from the liver, leading to congestion and necrosis.
![]() Severe infections: Systemic infections (sepsis) can sometimes contribute to liver damage.
Severe infections: Systemic infections (sepsis) can sometimes contribute to liver damage.
Types of Hepatic Necrosis:
Hepatic necrosis can be classified based on the pattern and extent of cell death:
![]() Zonal necrosis: Necrosis affects a specific zone of the liver lobule (the functional unit of the liver). Common patterns include:
Zonal necrosis: Necrosis affects a specific zone of the liver lobule (the functional unit of the liver). Common patterns include:![]()

![]() Centrilobular necrosis: Necrosis occurs around the central vein (zone 3), often associated with ischemia, toxins (like acetaminophen), or congestion (heart failure). This is the most common pattern.
Centrilobular necrosis: Necrosis occurs around the central vein (zone 3), often associated with ischemia, toxins (like acetaminophen), or congestion (heart failure). This is the most common pattern.![]()

![]() Midzonal necrosis: Necrosis occurs in the mid-zone (zone 2).
Midzonal necrosis: Necrosis occurs in the mid-zone (zone 2).![]()

![]() Periportal necrosis: Necrosis occurs around the portal triads (zone 1), less common and associated with toxins.
Periportal necrosis: Necrosis occurs around the portal triads (zone 1), less common and associated with toxins.
![]() Bridging necrosis: Necrosis connects different zones of the liver, such as central veins to portal triads. It's a more severe form and indicates more extensive liver damage.
Bridging necrosis: Necrosis connects different zones of the liver, such as central veins to portal triads. It's a more severe form and indicates more extensive liver damage.
![]() Massive necrosis: Necrosis affects large areas of the liver, leading to widespread liver failure. This is a very severe form.
Massive necrosis: Necrosis affects large areas of the liver, leading to widespread liver failure. This is a very severe form.
![]() Focal necrosis: Scattered areas of cell death throughout the liver.
Focal necrosis: Scattered areas of cell death throughout the liver.
Symptoms of Hepatic Necrosis:
Symptoms can vary depending on the severity and cause of the necrosis. They may include:
![]() Jaundice: Yellowing of the skin and eyes due to elevated bilirubin levels.
Jaundice: Yellowing of the skin and eyes due to elevated bilirubin levels.
![]() Abdominal pain: Especially in the upper right quadrant.
Abdominal pain: Especially in the upper right quadrant.
![]() Nausea and vomiting:
Nausea and vomiting:
![]() Fatigue:
Fatigue:
![]() Loss of appetite:
Loss of appetite:
![]() Dark urine:
Dark urine:
![]() Pale stools:
Pale stools:
![]() Swelling in the abdomen (ascites): Due to fluid accumulation.
Swelling in the abdomen (ascites): Due to fluid accumulation.
![]() Confusion or mental changes (hepatic encephalopathy): Due to the liver's inability to remove toxins from the blood.
Confusion or mental changes (hepatic encephalopathy): Due to the liver's inability to remove toxins from the blood.
![]() Bleeding or bruising easily: Due to impaired clotting factor production.
Bleeding or bruising easily: Due to impaired clotting factor production.
Diagnosis:
Diagnosis typically involves:
![]() Liver function tests (LFTs): Blood tests to assess liver enzyme levels (e.g., ALT, AST, alkaline phosphatase, bilirubin). Elevated levels indicate liver damage.
Liver function tests (LFTs): Blood tests to assess liver enzyme levels (e.g., ALT, AST, alkaline phosphatase, bilirubin). Elevated levels indicate liver damage.
![]() Coagulation studies: To assess the liver's ability to produce clotting factors.
Coagulation studies: To assess the liver's ability to produce clotting factors.
![]() Viral hepatitis testing: To rule out viral infections.
Viral hepatitis testing: To rule out viral infections.
![]() Drug and toxin screening: To identify potential causative agents.
Drug and toxin screening: To identify potential causative agents.
![]() Imaging studies: Ultrasound, CT scan, or MRI to visualize the liver and identify any abnormalities.
Imaging studies: Ultrasound, CT scan, or MRI to visualize the liver and identify any abnormalities.
![]() Liver biopsy: A small sample of liver tissue is taken and examined under a microscope to confirm the diagnosis and determine the extent and pattern of necrosis.
Liver biopsy: A small sample of liver tissue is taken and examined under a microscope to confirm the diagnosis and determine the extent and pattern of necrosis.
Treatment:
Treatment depends on the underlying cause of the hepatic necrosis. It may include:
![]() Supportive care: Includes managing symptoms, providing nutritional support, and preventing complications.
Supportive care: Includes managing symptoms, providing nutritional support, and preventing complications.
![]() Discontinuation of offending agents: Stopping any drugs or toxins that are causing the liver damage.
Discontinuation of offending agents: Stopping any drugs or toxins that are causing the liver damage.
![]() Antiviral medications: For viral hepatitis.
Antiviral medications: For viral hepatitis.
![]() Immunosuppressants: For autoimmune hepatitis.
Immunosuppressants: For autoimmune hepatitis.
![]() Chelation therapy: For Wilson's disease (to remove excess copper).
Chelation therapy: For Wilson's disease (to remove excess copper).
![]() Liver transplantation: May be necessary in severe cases of liver failure.
Liver transplantation: May be necessary in severe cases of liver failure.
Prognosis:
The prognosis depends on the severity of the necrosis, the underlying cause, and the patient's overall health. Mild necrosis may resolve with treatment, while severe necrosis can lead to liver failure and death.
In summary, hepatic necrosis is a serious condition characterized by the death of liver cells. It can be caused by a variety of factors, including drugs, viruses, toxins, and ischemia. Diagnosis involves blood tests, imaging studies, and sometimes a liver biopsy. Treatment depends on the underlying cause and may include supportive care, medications, or liver transplantation.