Histidinemia
Published: 18 Jun 2025
ICD9: 270.5 ICD10: E70.40 ICD11: 5C50.20
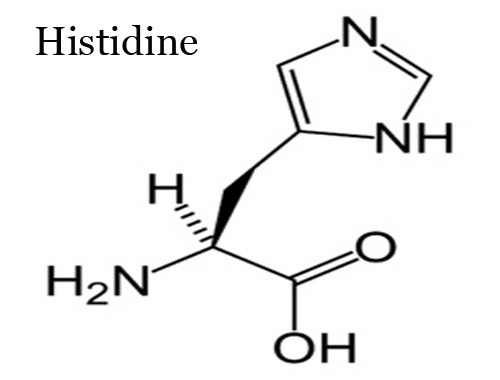
Histidinemia is a rare inherited metabolic disorder caused by a deficiency of the enzyme histidase (also known as histidine ammonia-lyase).
This enzyme is essential for the breakdown of the amino acid histidine.
Here's a breakdown of what that means:
![]() Inherited Metabolic Disorder: Histidinemia is a genetic condition passed down from parents to their children. It disrupts normal chemical processes (metabolism) in the body.
Inherited Metabolic Disorder: Histidinemia is a genetic condition passed down from parents to their children. It disrupts normal chemical processes (metabolism) in the body.
![]() Histidase (Histidine Ammonia-Lyase) Deficiency: The core problem is a lack of or a malfunctioning histidase enzyme. This enzyme is normally responsible for converting histidine into urocanic acid, the first step in the breakdown of histidine.
Histidase (Histidine Ammonia-Lyase) Deficiency: The core problem is a lack of or a malfunctioning histidase enzyme. This enzyme is normally responsible for converting histidine into urocanic acid, the first step in the breakdown of histidine.
![]() Histidine Buildup: Because the enzyme isn't working properly, histidine accumulates in the blood, urine, and cerebrospinal fluid.
Histidine Buildup: Because the enzyme isn't working properly, histidine accumulates in the blood, urine, and cerebrospinal fluid.
Effects and Symptoms:
![]() For many years, histidinemia was thought to cause intellectual disability and speech problems. However, it is now generally considered to be a benign condition for the vast majority of affected individuals. Most people with histidinemia do not experience any noticeable symptoms or health problems.
For many years, histidinemia was thought to cause intellectual disability and speech problems. However, it is now generally considered to be a benign condition for the vast majority of affected individuals. Most people with histidinemia do not experience any noticeable symptoms or health problems.
![]() Historical Concerns: In the past, there were reports of developmental delays, learning difficulties, and speech problems in some individuals diagnosed with histidinemia. However, it is now believed that these issues were likely unrelated to the condition itself or were due to other factors.
Historical Concerns: In the past, there were reports of developmental delays, learning difficulties, and speech problems in some individuals diagnosed with histidinemia. However, it is now believed that these issues were likely unrelated to the condition itself or were due to other factors.
![]() Rare, Possible Symptoms (Controversial): Very rarely, and controversially, some researchers have suggested a possible link between histidinemia and:
Rare, Possible Symptoms (Controversial): Very rarely, and controversially, some researchers have suggested a possible link between histidinemia and:![]()

![]() Speech delay or articulation problems (although this is debated)
Speech delay or articulation problems (although this is debated)![]()

![]() Mild developmental delays in some cases
Mild developmental delays in some cases
Diagnosis:
![]() Newborn screening: Histidinemia is often detected through routine newborn screening programs that test for various metabolic disorders. This screening measures histidine levels in the blood.
Newborn screening: Histidinemia is often detected through routine newborn screening programs that test for various metabolic disorders. This screening measures histidine levels in the blood.
![]() Elevated histidine levels: If the initial screening shows elevated histidine, further testing (e.g., blood tests, urine tests, enzyme assays) is done to confirm the diagnosis and rule out other conditions. Genetic testing can also be used to identify specific mutations in the *HAL* gene, which encodes the histidase enzyme.
Elevated histidine levels: If the initial screening shows elevated histidine, further testing (e.g., blood tests, urine tests, enzyme assays) is done to confirm the diagnosis and rule out other conditions. Genetic testing can also be used to identify specific mutations in the *HAL* gene, which encodes the histidase enzyme.
Treatment:
![]() Dietary Restriction (Historically used, now generally not recommended): Historically, a low-histidine diet was recommended for infants and children diagnosed with histidinemia. However, because most people with the condition are asymptomatic and the long-term benefits of dietary restriction are uncertain, dietary treatment is generally no longer recommended.
Dietary Restriction (Historically used, now generally not recommended): Historically, a low-histidine diet was recommended for infants and children diagnosed with histidinemia. However, because most people with the condition are asymptomatic and the long-term benefits of dietary restriction are uncertain, dietary treatment is generally no longer recommended.
![]() Monitoring: Because the condition is usually harmless, the primary approach is monitoring. Doctors may monitor histidine levels to ensure they aren't excessively high.
Monitoring: Because the condition is usually harmless, the primary approach is monitoring. Doctors may monitor histidine levels to ensure they aren't excessively high.
Important Considerations:
![]() Variability: The severity of histidinemia can vary.
Variability: The severity of histidinemia can vary.
![]() Research and Understanding: Research into histidinemia is ongoing to better understand the condition and its potential effects.
Research and Understanding: Research into histidinemia is ongoing to better understand the condition and its potential effects.
![]() Consult a Specialist: If you or your child has been diagnosed with histidinemia, it is essential to consult with a metabolic specialist or geneticist. They can provide the most up-to-date information, discuss potential risks and benefits of treatment, and help you make informed decisions about your care.
Consult a Specialist: If you or your child has been diagnosed with histidinemia, it is essential to consult with a metabolic specialist or geneticist. They can provide the most up-to-date information, discuss potential risks and benefits of treatment, and help you make informed decisions about your care.
In summary, histidinemia is typically a benign metabolic condition resulting from a deficiency in histidase. Most individuals with histidinemia are asymptomatic, and treatment is usually not required. However, diagnosis and monitoring are important to ensure that any potential issues are addressed.