Hyperammonemia
Published: 18 Jun 2025
ICD9: 270.6 ICD10: E72.20 ICD11: 5C50.AY
Hyperammonemia refers to a metabolic condition characterized by elevated levels of ammonia in the blood.
Here's a breakdown:
![]() Ammonia (NH3): A toxic waste product produced during the metabolism of proteins and amino acids.
Ammonia (NH3): A toxic waste product produced during the metabolism of proteins and amino acids.
![]() Normal Process: Normally, ammonia is transported to the liver, where it's converted into urea through the urea cycle. Urea is then excreted by the kidneys in urine.
Normal Process: Normally, ammonia is transported to the liver, where it's converted into urea through the urea cycle. Urea is then excreted by the kidneys in urine.
![]() Hyperammonemia's problem: In hyperammonemia, this process is disrupted, leading to an accumulation of ammonia in the bloodstream.
Hyperammonemia's problem: In hyperammonemia, this process is disrupted, leading to an accumulation of ammonia in the bloodstream.
Causes of Hyperammonemia:
Hyperammonemia can be caused by a variety of factors, including:
![]() Liver Disease: Liver cirrhosis, hepatitis, and other liver disorders can impair the liver's ability to process ammonia. This is a common cause in adults.
Liver Disease: Liver cirrhosis, hepatitis, and other liver disorders can impair the liver's ability to process ammonia. This is a common cause in adults.
![]() Genetic Disorders: Urea cycle disorders are a group of inherited genetic conditions that affect the enzymes involved in the urea cycle. These are typically diagnosed in infancy or early childhood. Examples include:
Genetic Disorders: Urea cycle disorders are a group of inherited genetic conditions that affect the enzymes involved in the urea cycle. These are typically diagnosed in infancy or early childhood. Examples include:![]()

![]() Ornithine transcarbamylase deficiency (OTCD)
Ornithine transcarbamylase deficiency (OTCD)![]()

![]() Carbamoyl phosphate synthetase I deficiency (CPS1)
Carbamoyl phosphate synthetase I deficiency (CPS1)![]()

![]() Argininosuccinate synthetase deficiency (ASS)
Argininosuccinate synthetase deficiency (ASS)![]()

![]() Argininosuccinate lyase deficiency (ASL)
Argininosuccinate lyase deficiency (ASL)![]()

![]() Arginase deficiency (ARG)
Arginase deficiency (ARG)
![]() Medications: Some medications, such as valproic acid (an anti-seizure medication), can sometimes cause hyperammonemia.
Medications: Some medications, such as valproic acid (an anti-seizure medication), can sometimes cause hyperammonemia.
![]() Infections: Some infections, especially those that affect the liver, can lead to hyperammonemia.
Infections: Some infections, especially those that affect the liver, can lead to hyperammonemia.
![]() Kidney Failure: Impaired kidney function can contribute to ammonia buildup, although this is less direct than liver dysfunction.
Kidney Failure: Impaired kidney function can contribute to ammonia buildup, although this is less direct than liver dysfunction.
![]() Reye's Syndrome: A rare but serious condition that primarily affects children, often following a viral illness, and can cause liver and brain damage leading to hyperammonemia. Aspirin use during a viral illness is a risk factor.
Reye's Syndrome: A rare but serious condition that primarily affects children, often following a viral illness, and can cause liver and brain damage leading to hyperammonemia. Aspirin use during a viral illness is a risk factor.
![]() Total Parenteral Nutrition (TPN): Prolonged intravenous feeding can sometimes lead to hyperammonemia, especially in patients with underlying metabolic vulnerabilities.
Total Parenteral Nutrition (TPN): Prolonged intravenous feeding can sometimes lead to hyperammonemia, especially in patients with underlying metabolic vulnerabilities.
![]() Certain Cancers: Some cancers can disrupt metabolic processes and contribute to hyperammonemia.
Certain Cancers: Some cancers can disrupt metabolic processes and contribute to hyperammonemia.
Symptoms of Hyperammonemia:
Symptoms can vary depending on the severity and underlying cause, but may include:
![]() In infants:
In infants:![]()

![]() Lethargy
Lethargy![]()

![]() Poor feeding
Poor feeding![]()

![]() Vomiting
Vomiting![]()

![]() Irritability
Irritability![]()

![]() Seizures
Seizures![]()

![]() Coma
Coma
![]() In older children and adults:
In older children and adults:![]()

![]() Confusion
Confusion![]()

![]() Disorientation
Disorientation![]()

![]() Slurred speech
Slurred speech![]()

![]() Personality changes
Personality changes![]()

![]() Tremors
Tremors![]()

![]() Ataxia (lack of coordination)
Ataxia (lack of coordination)![]()

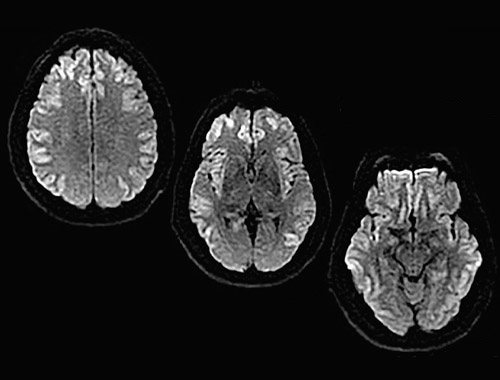
![]() Encephalopathy (brain dysfunction)
Encephalopathy (brain dysfunction)![]()

![]() Lethargy
Lethargy![]()

![]() Coma
Coma
Diagnosis:
Hyperammonemia is diagnosed by measuring the ammonia level in the blood. Further testing is done to determine the underlying cause, such as liver function tests, genetic testing, and imaging studies.
Treatment:
Treatment depends on the cause and severity of hyperammonemia. The primary goals are to lower ammonia levels and prevent further brain damage. Treatments may include:
![]() Dietary management: Restricting protein intake.
Dietary management: Restricting protein intake.
![]() Medications:
Medications:![]()

![]() Lactulose (helps remove ammonia from the body through the stool)
Lactulose (helps remove ammonia from the body through the stool)![]()

![]() Sodium benzoate and sodium phenylacetate (help remove ammonia from the body through the urine)
Sodium benzoate and sodium phenylacetate (help remove ammonia from the body through the urine)![]()

![]() Ammonium scavengers (e.g., carglumic acid)
Ammonium scavengers (e.g., carglumic acid)
![]() Hemodialysis or hemofiltration: To remove ammonia from the blood in severe cases.
Hemodialysis or hemofiltration: To remove ammonia from the blood in severe cases.
![]() Liver transplant: In cases of severe liver disease.
Liver transplant: In cases of severe liver disease.
![]() Treating the underlying cause: Addressing the underlying medical condition that is causing the hyperammonemia.
Treating the underlying cause: Addressing the underlying medical condition that is causing the hyperammonemia.
Why is it important?
Hyperammonemia is a serious condition because ammonia is toxic to the brain. Elevated ammonia levels can cause brain damage, leading to neurological problems, coma, and even death. Prompt diagnosis and treatment are crucial to minimize the risk of long-term complications.