Hyperparathyroidism
Published: 18 Jun 2025
ICD9: 252.00 ICD10: E21.3 ICD11: 5A51
Hyperparathyroidism is a condition where the parathyroid glands produce too much parathyroid hormone (PTH).
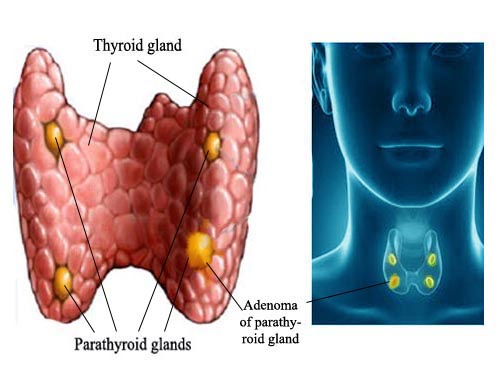
The parathyroid glands are four small glands located in the neck, near the thyroid gland. They play a crucial role in regulating calcium levels in the blood.
Here's a breakdown of what that means:
![]() Parathyroid glands: These glands are about the size of a grain of rice.
Parathyroid glands: These glands are about the size of a grain of rice.
![]() Parathyroid hormone (PTH): PTH is the hormone produced by the parathyroid glands. Its primary function is to increase calcium levels in the blood. It does this through several mechanisms:
Parathyroid hormone (PTH): PTH is the hormone produced by the parathyroid glands. Its primary function is to increase calcium levels in the blood. It does this through several mechanisms:![]()

![]() Stimulating bone resorption: PTH signals bone cells to release calcium from the bones into the bloodstream.
Stimulating bone resorption: PTH signals bone cells to release calcium from the bones into the bloodstream.![]()

![]() Increasing calcium absorption in the intestines: PTH indirectly increases calcium absorption from food by stimulating the kidneys to produce active vitamin D, which is essential for calcium absorption.
Increasing calcium absorption in the intestines: PTH indirectly increases calcium absorption from food by stimulating the kidneys to produce active vitamin D, which is essential for calcium absorption.![]()

![]() Reducing calcium excretion in the kidneys: PTH tells the kidneys to conserve calcium and excrete less of it in the urine.
Reducing calcium excretion in the kidneys: PTH tells the kidneys to conserve calcium and excrete less of it in the urine.
So, in hyperparathyroidism, the parathyroid glands are overactive and produce too much PTH. This leads to elevated levels of calcium in the blood (hypercalcemia).
Types of Hyperparathyroidism:
![]() Primary Hyperparathyroidism: This is the most common type. It's usually caused by a problem within one or more of the parathyroid glands themselves. The most common causes are:
Primary Hyperparathyroidism: This is the most common type. It's usually caused by a problem within one or more of the parathyroid glands themselves. The most common causes are:![]()

![]() Parathyroid adenoma: A benign (non-cancerous) tumor on one of the parathyroid glands is the most frequent culprit.
Parathyroid adenoma: A benign (non-cancerous) tumor on one of the parathyroid glands is the most frequent culprit.![]()

![]() Parathyroid hyperplasia: Enlargement of all four parathyroid glands. This is more common in inherited conditions.
Parathyroid hyperplasia: Enlargement of all four parathyroid glands. This is more common in inherited conditions.![]()

![]() Parathyroid carcinoma: Rarely, hyperparathyroidism is caused by a cancerous tumor on a parathyroid gland.
Parathyroid carcinoma: Rarely, hyperparathyroidism is caused by a cancerous tumor on a parathyroid gland.
![]() Secondary Hyperparathyroidism: This is caused by another medical condition that leads to low calcium levels in the blood. The parathyroid glands then try to compensate by producing more PTH to raise calcium levels. Common causes include:
Secondary Hyperparathyroidism: This is caused by another medical condition that leads to low calcium levels in the blood. The parathyroid glands then try to compensate by producing more PTH to raise calcium levels. Common causes include:![]()

![]() Chronic kidney disease: The kidneys play a key role in activating vitamin D and removing phosphorus from the body. Kidney disease can disrupt these processes, leading to low calcium and high phosphorus levels, which stimulate PTH production.
Chronic kidney disease: The kidneys play a key role in activating vitamin D and removing phosphorus from the body. Kidney disease can disrupt these processes, leading to low calcium and high phosphorus levels, which stimulate PTH production.![]()

![]() Vitamin D deficiency: Vitamin D is essential for calcium absorption from the intestines. If you don't have enough vitamin D, your body can't absorb calcium properly, leading to low calcium levels and stimulating PTH production.
Vitamin D deficiency: Vitamin D is essential for calcium absorption from the intestines. If you don't have enough vitamin D, your body can't absorb calcium properly, leading to low calcium levels and stimulating PTH production.![]()

![]() Calcium deficiency: Inadequate calcium intake can also lead to secondary hyperparathyroidism.
Calcium deficiency: Inadequate calcium intake can also lead to secondary hyperparathyroidism.
![]() Tertiary Hyperparathyroidism: This can occur in people who have had long-standing secondary hyperparathyroidism, often due to chronic kidney disease. Over time, the parathyroid glands become autonomous and begin producing excessive PTH even after the underlying condition is treated and calcium levels are normalized.
Tertiary Hyperparathyroidism: This can occur in people who have had long-standing secondary hyperparathyroidism, often due to chronic kidney disease. Over time, the parathyroid glands become autonomous and begin producing excessive PTH even after the underlying condition is treated and calcium levels are normalized.
Symptoms:
Many people with hyperparathyroidism have no symptoms at all, especially in the early stages. When symptoms do occur, they can be vague and nonspecific. However, as calcium levels rise, symptoms may include:
![]() Bone pain and fractures: Excess PTH can weaken bones, making them more prone to fractures.
Bone pain and fractures: Excess PTH can weaken bones, making them more prone to fractures.
![]() Kidney stones: High calcium levels in the urine can lead to the formation of kidney stones.
Kidney stones: High calcium levels in the urine can lead to the formation of kidney stones.
![]() Excessive urination and thirst: High calcium can interfere with the kidneys' ability to concentrate urine.
Excessive urination and thirst: High calcium can interfere with the kidneys' ability to concentrate urine.
![]() Fatigue, weakness, and muscle aches:
Fatigue, weakness, and muscle aches:
![]() Depression, anxiety, and memory problems:
Depression, anxiety, and memory problems:
![]() Gastrointestinal problems: Nausea, vomiting, constipation, and abdominal pain.
Gastrointestinal problems: Nausea, vomiting, constipation, and abdominal pain.
![]() Heart problems: In rare cases, hypercalcemia can lead to irregular heart rhythms.
Heart problems: In rare cases, hypercalcemia can lead to irregular heart rhythms.
Diagnosis:
Hyperparathyroidism is usually diagnosed through blood tests that measure:
![]() Parathyroid hormone (PTH) levels: Elevated PTH levels are a key indicator of hyperparathyroidism.
Parathyroid hormone (PTH) levels: Elevated PTH levels are a key indicator of hyperparathyroidism.
![]() Calcium levels: Elevated calcium levels (hypercalcemia) are another important finding.
Calcium levels: Elevated calcium levels (hypercalcemia) are another important finding.
![]() Phosphorus levels: Phosphorus levels may be low in primary hyperparathyroidism.
Phosphorus levels: Phosphorus levels may be low in primary hyperparathyroidism.
![]() Vitamin D levels: Vitamin D levels are checked to rule out vitamin D deficiency as a cause of secondary hyperparathyroidism.
Vitamin D levels: Vitamin D levels are checked to rule out vitamin D deficiency as a cause of secondary hyperparathyroidism.
![]() Kidney function tests: These tests assess kidney health.
Kidney function tests: These tests assess kidney health.
If blood tests suggest hyperparathyroidism, further tests may be performed to determine the cause and severity of the condition. These tests may include:
![]() Sestamibi scan (parathyroid scan): This imaging test helps locate overactive parathyroid glands.
Sestamibi scan (parathyroid scan): This imaging test helps locate overactive parathyroid glands.
![]() Ultrasound: Ultrasound can be used to visualize the parathyroid glands.
Ultrasound: Ultrasound can be used to visualize the parathyroid glands.
![]() Bone density test (DEXA scan): This test measures bone mineral density to assess the risk of osteoporosis.
Bone density test (DEXA scan): This test measures bone mineral density to assess the risk of osteoporosis.
Treatment:
Treatment for hyperparathyroidism depends on the type and severity of the condition, as well as the patient's overall health and symptoms.
![]() Primary Hyperparathyroidism:
Primary Hyperparathyroidism:![]()

![]() Surgery: The most common and effective treatment for primary hyperparathyroidism is surgery to remove the overactive parathyroid gland(s) (parathyroidectomy). This is often done using minimally invasive techniques.
Surgery: The most common and effective treatment for primary hyperparathyroidism is surgery to remove the overactive parathyroid gland(s) (parathyroidectomy). This is often done using minimally invasive techniques.![]()

![]() Observation: In some cases, if calcium levels are only mildly elevated, symptoms are minimal, and the patient is at low risk of complications, observation with regular monitoring may be an option. However, surgery is generally recommended for most patients.
Observation: In some cases, if calcium levels are only mildly elevated, symptoms are minimal, and the patient is at low risk of complications, observation with regular monitoring may be an option. However, surgery is generally recommended for most patients.
![]() Secondary Hyperparathyroidism:
Secondary Hyperparathyroidism:![]()

![]() Treating the underlying cause: The primary focus is on addressing the underlying condition that is causing the low calcium levels, such as chronic kidney disease or vitamin D deficiency.
Treating the underlying cause: The primary focus is on addressing the underlying condition that is causing the low calcium levels, such as chronic kidney disease or vitamin D deficiency.![]()

![]() Vitamin D supplementation: Vitamin D supplements are often prescribed to raise calcium levels.
Vitamin D supplementation: Vitamin D supplements are often prescribed to raise calcium levels.![]()

![]() Calcium supplements: Calcium supplements may also be recommended.
Calcium supplements: Calcium supplements may also be recommended.![]()

![]() Phosphate binders: In people with chronic kidney disease, phosphate binders can help lower phosphorus levels, which can contribute to secondary hyperparathyroidism.
Phosphate binders: In people with chronic kidney disease, phosphate binders can help lower phosphorus levels, which can contribute to secondary hyperparathyroidism.![]()

![]() Calcimimetic medications: These medications (e.g., cinacalcet) can help lower PTH levels by increasing the sensitivity of the parathyroid glands to calcium.
Calcimimetic medications: These medications (e.g., cinacalcet) can help lower PTH levels by increasing the sensitivity of the parathyroid glands to calcium.
![]() Tertiary Hyperparathyroidism:
Tertiary Hyperparathyroidism:![]()

![]() Parathyroidectomy: Surgery to remove the overactive parathyroid glands is often necessary, as the glands have become autonomous and no longer respond to medical management.
Parathyroidectomy: Surgery to remove the overactive parathyroid glands is often necessary, as the glands have become autonomous and no longer respond to medical management.
Complications of Untreated Hyperparathyroidism:
If left untreated, hyperparathyroidism can lead to serious complications, including:
![]() Osteoporosis and fractures:
Osteoporosis and fractures:
![]() Kidney stones and kidney damage:
Kidney stones and kidney damage:
![]() Cardiovascular disease:
Cardiovascular disease:
![]() High blood pressure:
High blood pressure:
![]() Peptic ulcers:
Peptic ulcers:
![]() Pancreatitis:
Pancreatitis:
![]() Neurological problems:
Neurological problems:
In summary, hyperparathyroidism is a condition characterized by overproduction of parathyroid hormone, leading to elevated blood calcium levels. Early diagnosis and treatment are crucial to prevent serious complications. If you suspect you might have hyperparathyroidism, it's important to consult a doctor for evaluation and management.