Hypogonadism in male (Testicular hypofunction)
Published: 18 Jun 2025
ICD9: 257.2 ICD10: E29.1 ICD11: 5A81.1
Hypogonadism in males, also known as testicular hypofunction, is a condition in which the testes (testicles) don't produce enough testosterone, sperm, or both.
Testosterone is the primary male sex hormone, crucial for developing male characteristics and maintaining various bodily functions. Sperm production is essential for fertility.
Here's a breakdown of key aspects:
What it means:
![]() Insufficient Testosterone Production: The testicles don't produce enough testosterone. Testosterone is vital for:
Insufficient Testosterone Production: The testicles don't produce enough testosterone. Testosterone is vital for:![]()

![]() Sexual development: Growth of penis and testes during puberty, deepening of voice, growth of facial and body hair.
Sexual development: Growth of penis and testes during puberty, deepening of voice, growth of facial and body hair.![]()

![]() Sexual function: Libido (sex drive), erectile function.
Sexual function: Libido (sex drive), erectile function.![]()

![]() Muscle mass and strength: Testosterone helps build and maintain muscle.
Muscle mass and strength: Testosterone helps build and maintain muscle.![]()

![]() Bone density: Important for strong bones.
Bone density: Important for strong bones.![]()

![]() Red blood cell production: Testosterone stimulates the bone marrow to produce red blood cells.
Red blood cell production: Testosterone stimulates the bone marrow to produce red blood cells.![]()

![]() Energy levels and mood: Impacts energy levels, mood, and cognitive function.
Energy levels and mood: Impacts energy levels, mood, and cognitive function.
![]() Insufficient Sperm Production: The testicles don't produce enough sperm. This can lead to:
Insufficient Sperm Production: The testicles don't produce enough sperm. This can lead to:![]()

![]() Infertility: Difficulty conceiving a child.
Infertility: Difficulty conceiving a child.
Types of Hypogonadism:
Hypogonadism is classified into two main types, based on the underlying cause:
![]() Primary Hypogonadism (Testicular Failure): The problem lies directly within the testicles themselves. The testicles are unable to produce sufficient testosterone, even when stimulated by the brain. Common causes include:
Primary Hypogonadism (Testicular Failure): The problem lies directly within the testicles themselves. The testicles are unable to produce sufficient testosterone, even when stimulated by the brain. Common causes include:![]()

![]() Klinefelter syndrome: A genetic condition where a male has an extra X chromosome (XXY instead of XY).
Klinefelter syndrome: A genetic condition where a male has an extra X chromosome (XXY instead of XY).![]()

![]() Undescended testicles (cryptorchidism): Testicles that don't descend into the scrotum during development.
Undescended testicles (cryptorchidism): Testicles that don't descend into the scrotum during development.![]()

![]() Mumps orchitis: Inflammation of the testicles caused by the mumps virus.
Mumps orchitis: Inflammation of the testicles caused by the mumps virus.![]()

![]() Testicular injury or trauma: Damage to the testicles.
Testicular injury or trauma: Damage to the testicles.![]()

![]() Cancer treatment (chemotherapy or radiation): Can damage the testicles.
Cancer treatment (chemotherapy or radiation): Can damage the testicles.![]()

![]() Certain autoimmune diseases: Can attack the testicles.
Certain autoimmune diseases: Can attack the testicles.![]()

![]() Varicocele: Enlarged veins in the scrotum, which can sometimes affect testicular function.
Varicocele: Enlarged veins in the scrotum, which can sometimes affect testicular function.![]()

![]() Aging: Testosterone levels naturally decline with age.
Aging: Testosterone levels naturally decline with age.![]()

![]() Noonan syndrome: A genetic disorder that can affect the development of many parts of the body, including the testicles.
Noonan syndrome: A genetic disorder that can affect the development of many parts of the body, including the testicles.
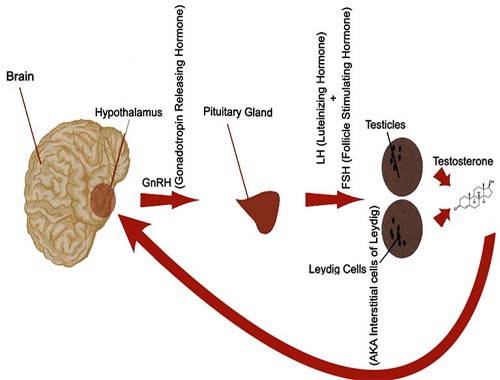
![]() Secondary Hypogonadism (Central Hypogonadism): The problem originates in the brain, specifically the hypothalamus or pituitary gland. These glands are responsible for producing hormones (luteinizing hormone - LH and follicle-stimulating hormone - FSH) that stimulate the testicles to produce testosterone and sperm. Causes include:
Secondary Hypogonadism (Central Hypogonadism): The problem originates in the brain, specifically the hypothalamus or pituitary gland. These glands are responsible for producing hormones (luteinizing hormone - LH and follicle-stimulating hormone - FSH) that stimulate the testicles to produce testosterone and sperm. Causes include:![]()

![]() Pituitary tumors: Can disrupt hormone production.
Pituitary tumors: Can disrupt hormone production.![]()

![]() Kallmann syndrome: A genetic condition affecting the hypothalamus, leading to delayed or absent puberty and impaired sense of smell.
Kallmann syndrome: A genetic condition affecting the hypothalamus, leading to delayed or absent puberty and impaired sense of smell.![]()

![]() Head trauma or brain injury: Can damage the hypothalamus or pituitary gland.
Head trauma or brain injury: Can damage the hypothalamus or pituitary gland.![]()

![]() Certain medications: Opioids, anabolic steroids, and some other medications can suppress testosterone production.
Certain medications: Opioids, anabolic steroids, and some other medications can suppress testosterone production.![]()

![]() Obesity: Excess body fat can interfere with hormone regulation.
Obesity: Excess body fat can interfere with hormone regulation.![]()

![]() HIV/AIDS: Can affect the hypothalamus or pituitary gland.
HIV/AIDS: Can affect the hypothalamus or pituitary gland.![]()

![]() Inflammatory diseases: Sarcoidosis, tuberculosis, and histiocytosis.
Inflammatory diseases: Sarcoidosis, tuberculosis, and histiocytosis.![]()

![]() Hemochromatosis: A condition where the body absorbs too much iron.
Hemochromatosis: A condition where the body absorbs too much iron.![]()

![]() Hypothalamic dysfunction: Problems with the hypothalamus's ability to release gonadotropin-releasing hormone (GnRH).
Hypothalamic dysfunction: Problems with the hypothalamus's ability to release gonadotropin-releasing hormone (GnRH).
Symptoms:
The symptoms of hypogonadism vary depending on the age of onset and the severity of the testosterone deficiency.
![]() In babies:
In babies:![]()

![]() Ambiguous genitalia
Ambiguous genitalia![]()

![]() Small penis or testicles
Small penis or testicles![]()

![]() Delayed or absent puberty
Delayed or absent puberty
![]() In adolescent males:
In adolescent males:![]()

![]() Delayed or incomplete puberty
Delayed or incomplete puberty![]()

![]() Lack of muscle development
Lack of muscle development![]()

![]() Little or no body hair
Little or no body hair![]()

![]() High-pitched voice
High-pitched voice![]()

![]() Enlarged breasts (gynecomastia)
Enlarged breasts (gynecomastia)![]()

![]() Small penis and testicles
Small penis and testicles![]()

![]() Long arms and legs relative to the trunk
Long arms and legs relative to the trunk
![]() In adult males:
In adult males:![]()

![]() Decreased libido (sex drive)
Decreased libido (sex drive)![]()

![]() Erectile dysfunction (ED)
Erectile dysfunction (ED)![]()

![]() Infertility
Infertility![]()

![]() Loss of body hair
Loss of body hair![]()

![]() Decreased muscle mass and strength
Decreased muscle mass and strength![]()

![]() Increased body fat
Increased body fat![]()

![]() Gynecomastia (enlarged breasts)
Gynecomastia (enlarged breasts)![]()

![]() Fatigue
Fatigue![]()

![]() Depression or mood changes
Depression or mood changes![]()

![]() Decreased bone density (osteoporosis), leading to increased risk of fractures
Decreased bone density (osteoporosis), leading to increased risk of fractures![]()

![]() Hot flashes
Hot flashes![]()

![]() Cognitive problems (difficulty concentrating, memory issues)
Cognitive problems (difficulty concentrating, memory issues)![]()

![]() Smaller testicles
Smaller testicles
Diagnosis:
![]() Physical Exam: A doctor will perform a physical exam, paying attention to the size and consistency of the testicles, body hair distribution, and presence of gynecomastia.
Physical Exam: A doctor will perform a physical exam, paying attention to the size and consistency of the testicles, body hair distribution, and presence of gynecomastia.
![]() Blood Tests:
Blood Tests:![]()

![]() Testosterone levels: Measuring testosterone levels in the blood is the primary diagnostic test. It's often measured in the morning, as testosterone levels are typically highest then. Multiple measurements may be needed.
Testosterone levels: Measuring testosterone levels in the blood is the primary diagnostic test. It's often measured in the morning, as testosterone levels are typically highest then. Multiple measurements may be needed.![]()

![]() Luteinizing hormone (LH) and follicle-stimulating hormone (FSH): These hormones help determine whether the problem is primary or secondary hypogonadism.
Luteinizing hormone (LH) and follicle-stimulating hormone (FSH): These hormones help determine whether the problem is primary or secondary hypogonadism.![]()

![]() *High LH and FSH with low testosterone* usually indicate primary hypogonadism (testicular failure). The brain is trying to stimulate the testicles, but they aren't responding.
*High LH and FSH with low testosterone* usually indicate primary hypogonadism (testicular failure). The brain is trying to stimulate the testicles, but they aren't responding.![]()

![]() *Low LH and FSH with low testosterone* usually indicate secondary hypogonadism (a problem with the hypothalamus or pituitary gland). The brain isn't sending the proper signals to the testicles.
*Low LH and FSH with low testosterone* usually indicate secondary hypogonadism (a problem with the hypothalamus or pituitary gland). The brain isn't sending the proper signals to the testicles.![]()

![]() Prolactin: Elevated prolactin levels can sometimes suppress testosterone production.
Prolactin: Elevated prolactin levels can sometimes suppress testosterone production.![]()

![]() Other hormone levels: Estradiol (a type of estrogen), SHBG (sex hormone-binding globulin) and others may be tested to provide more information.
Other hormone levels: Estradiol (a type of estrogen), SHBG (sex hormone-binding globulin) and others may be tested to provide more information.
![]() Semen Analysis: To evaluate sperm count and quality, especially if fertility is a concern.
Semen Analysis: To evaluate sperm count and quality, especially if fertility is a concern.
![]() Genetic Testing: May be performed to diagnose genetic conditions like Klinefelter syndrome.
Genetic Testing: May be performed to diagnose genetic conditions like Klinefelter syndrome.
![]() Imaging Studies: An MRI of the pituitary gland may be needed to look for tumors or other abnormalities if secondary hypogonadism is suspected.
Imaging Studies: An MRI of the pituitary gland may be needed to look for tumors or other abnormalities if secondary hypogonadism is suspected.
![]() Bone Density Test: To assess for osteoporosis.
Bone Density Test: To assess for osteoporosis.
Treatment:
The treatment for hypogonadism depends on the underlying cause and the individual's goals. The primary treatment focuses on restoring testosterone levels to normal.
![]() Testosterone Replacement Therapy (TRT): The most common treatment for hypogonadism. Testosterone can be administered in several forms:
Testosterone Replacement Therapy (TRT): The most common treatment for hypogonadism. Testosterone can be administered in several forms:![]()

![]() Injections: Testosterone enanthate or cypionate injected into a muscle every 1-4 weeks.
Injections: Testosterone enanthate or cypionate injected into a muscle every 1-4 weeks.![]()

![]() Topical gels: Applied daily to the skin.
Topical gels: Applied daily to the skin.![]()

![]() Patches: Applied to the skin every day.
Patches: Applied to the skin every day.![]()

![]() Oral medications: Testosterone undecanoate capsules (available in some countries). Older oral forms of testosterone are generally avoided due to liver toxicity.
Oral medications: Testosterone undecanoate capsules (available in some countries). Older oral forms of testosterone are generally avoided due to liver toxicity.![]()

![]() Nasal gels: Applied inside the nose.
Nasal gels: Applied inside the nose.![]()

![]() Buccal tablets: Adhered to the upper gum.
Buccal tablets: Adhered to the upper gum.![]()

![]() Testosterone pellets: Implanted under the skin every few months.
Testosterone pellets: Implanted under the skin every few months.![]()

![]() TRT aims to relieve symptoms, improve libido, erectile function, energy levels, muscle mass, bone density, and mood.*
TRT aims to relieve symptoms, improve libido, erectile function, energy levels, muscle mass, bone density, and mood.*![]()

![]() TRT is generally not recommended for men who desire fertility as it can suppress sperm production.*
TRT is generally not recommended for men who desire fertility as it can suppress sperm production.*
![]() Fertility Treatment: If fertility is desired, treatment options may include:
Fertility Treatment: If fertility is desired, treatment options may include:![]()

![]() Clomiphene citrate: A medication that stimulates the pituitary gland to release LH and FSH, which can improve testosterone and sperm production.
Clomiphene citrate: A medication that stimulates the pituitary gland to release LH and FSH, which can improve testosterone and sperm production.![]()

![]() Human chorionic gonadotropin (hCG): Mimics LH and can stimulate testosterone production in the testicles.
Human chorionic gonadotropin (hCG): Mimics LH and can stimulate testosterone production in the testicles.![]()

![]() Assisted reproductive technologies (ART): Such as in vitro fertilization (IVF).
Assisted reproductive technologies (ART): Such as in vitro fertilization (IVF).
![]() Treatment of Underlying Conditions: If hypogonadism is caused by a pituitary tumor, treatment may involve surgery, radiation therapy, or medication. Addressing other underlying conditions like obesity or certain medications can also help.
Treatment of Underlying Conditions: If hypogonadism is caused by a pituitary tumor, treatment may involve surgery, radiation therapy, or medication. Addressing other underlying conditions like obesity or certain medications can also help.
Important Considerations:
![]() Benefits and Risks of TRT: It's crucial to discuss the potential benefits and risks of testosterone replacement therapy with a doctor.
Benefits and Risks of TRT: It's crucial to discuss the potential benefits and risks of testosterone replacement therapy with a doctor.![]()

![]() Potential Benefits: Increased libido, improved erectile function, increased muscle mass and strength, increased bone density, improved energy levels, improved mood.
Potential Benefits: Increased libido, improved erectile function, increased muscle mass and strength, increased bone density, improved energy levels, improved mood.![]()

![]() Potential Risks: Acne, oily skin, breast enlargement (gynecomastia), sleep apnea, increased red blood cell count (polycythemia), prostate enlargement, potential worsening of pre-existing prostate cancer (rare), potential cardiovascular risks (controversial and still under investigation).
Potential Risks: Acne, oily skin, breast enlargement (gynecomastia), sleep apnea, increased red blood cell count (polycythemia), prostate enlargement, potential worsening of pre-existing prostate cancer (rare), potential cardiovascular risks (controversial and still under investigation).
![]() Monitoring: Men on testosterone replacement therapy need regular monitoring, including blood tests to check testosterone levels, red blood cell count, and prostate-specific antigen (PSA).
Monitoring: Men on testosterone replacement therapy need regular monitoring, including blood tests to check testosterone levels, red blood cell count, and prostate-specific antigen (PSA).
![]() Individualized Treatment: The best treatment approach is tailored to the individual's specific needs and goals.
Individualized Treatment: The best treatment approach is tailored to the individual's specific needs and goals.
![]() Consult a specialist: An endocrinologist or urologist is usually the best type of doctor to consult regarding hypogonadism.
Consult a specialist: An endocrinologist or urologist is usually the best type of doctor to consult regarding hypogonadism.
In summary, hypogonadism in males (testicular hypofunction) is a condition resulting from inadequate production of testosterone, sperm, or both. It can be caused by problems with the testicles themselves or with the brain structures that control testicular function. Diagnosis involves blood tests and a physical exam, and treatment options depend on the cause and the individual's goals.