Hypoparathyroidism
Published: 18 Jun 2025
ICD9: 252.1 ICD10: E20.9 ICD11: 5A50
Hypoparathyroidism is a rare condition in which the parathyroid glands don't produce enough parathyroid hormone (PTH).
Here's a breakdown:
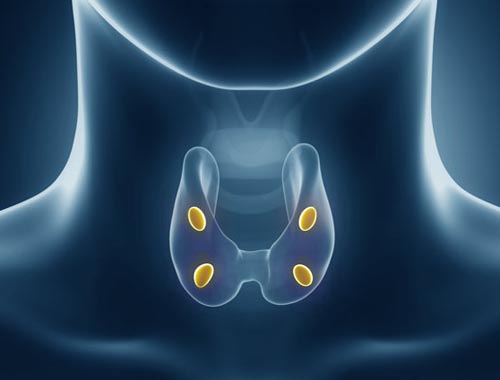
![]() Parathyroid Glands: These are four small glands located in the neck, behind the thyroid gland.
Parathyroid Glands: These are four small glands located in the neck, behind the thyroid gland.
![]() Parathyroid Hormone (PTH): This hormone plays a crucial role in regulating calcium and phosphorus levels in the blood. PTH works to increase calcium levels when they are too low.
Parathyroid Hormone (PTH): This hormone plays a crucial role in regulating calcium and phosphorus levels in the blood. PTH works to increase calcium levels when they are too low.
When PTH is deficient (hypoparathyroidism), calcium levels in the blood drop (hypocalcemia), and phosphorus levels rise (hyperphosphatemia).
Causes of Hypoparathyroidism:
![]() Surgery: The most common cause is damage to or removal of the parathyroid glands during thyroid or other neck surgery.
Surgery: The most common cause is damage to or removal of the parathyroid glands during thyroid or other neck surgery.
![]() Autoimmune Disease: The body's immune system attacks and destroys the parathyroid glands.
Autoimmune Disease: The body's immune system attacks and destroys the parathyroid glands.
![]() Genetic Factors: Certain inherited conditions can cause hypoparathyroidism. DiGeorge syndrome is one example.
Genetic Factors: Certain inherited conditions can cause hypoparathyroidism. DiGeorge syndrome is one example.
![]() Radiation Therapy: Radiation to the neck area can damage the parathyroid glands.
Radiation Therapy: Radiation to the neck area can damage the parathyroid glands.
![]() Magnesium Deficiency or Excess: Both too little and too much magnesium can interfere with PTH production or action.
Magnesium Deficiency or Excess: Both too little and too much magnesium can interfere with PTH production or action.
![]() Idiopathic: In some cases, the cause is unknown.
Idiopathic: In some cases, the cause is unknown.
Symptoms of Hypoparathyroidism:
Symptoms result from low calcium and high phosphorus levels. They can vary in severity and may include:
![]() Tingling or numbness: Particularly in the fingers, toes, and around the mouth.
Tingling or numbness: Particularly in the fingers, toes, and around the mouth.
![]() Muscle cramps, spasms, or twitching (tetany): This can be painful and even life-threatening.
Muscle cramps, spasms, or twitching (tetany): This can be painful and even life-threatening.
![]() Weakness and fatigue
Weakness and fatigue
![]() Seizures
Seizures
![]() Dry skin and brittle nails
Dry skin and brittle nails
![]() Hair loss
Hair loss
![]() Anxiety and depression
Anxiety and depression
![]() Confusion or memory problems
Confusion or memory problems
![]() Headaches
Headaches
![]() Abdominal pain
Abdominal pain
![]() Cataracts (over time)
Cataracts (over time)
Diagnosis:
Hypoparathyroidism is diagnosed based on:
![]() Blood tests: To measure calcium, phosphorus, and PTH levels. Low calcium, high phosphorus, and low or inappropriately normal PTH levels are indicative of the condition.
Blood tests: To measure calcium, phosphorus, and PTH levels. Low calcium, high phosphorus, and low or inappropriately normal PTH levels are indicative of the condition.
![]() Urine tests: To assess calcium excretion.
Urine tests: To assess calcium excretion.
![]() Medical history and physical exam: To identify potential causes.
Medical history and physical exam: To identify potential causes.
![]() Genetic testing: May be done to identify inherited forms.
Genetic testing: May be done to identify inherited forms.
Treatment:
The goal of treatment is to restore normal calcium and phosphorus levels and relieve symptoms. Treatment typically involves:
![]() Calcium supplements: Taken orally, often multiple times per day.
Calcium supplements: Taken orally, often multiple times per day.
![]() Vitamin D supplements: Vitamin D helps the body absorb calcium. Calcitriol (an active form of vitamin D) is often used.
Vitamin D supplements: Vitamin D helps the body absorb calcium. Calcitriol (an active form of vitamin D) is often used.
![]() Magnesium supplements: If magnesium deficiency is present.
Magnesium supplements: If magnesium deficiency is present.
![]() Thiazide diuretics: These medications can help the kidneys retain calcium.
Thiazide diuretics: These medications can help the kidneys retain calcium.
![]() Recombinant Human PTH (Natpara): Is an injection of synthetic PTH. However, its use has been limited due to concerns. It is not available in many countries. It is typically reserved for people who are not well controlled with calcium and vitamin D alone.
Recombinant Human PTH (Natpara): Is an injection of synthetic PTH. However, its use has been limited due to concerns. It is not available in many countries. It is typically reserved for people who are not well controlled with calcium and vitamin D alone.
![]() Diet: A diet high in calcium and low in phosphorus may be recommended. Avoiding high-phosphorus foods like dairy products, processed foods, and carbonated beverages is often advised.
Diet: A diet high in calcium and low in phosphorus may be recommended. Avoiding high-phosphorus foods like dairy products, processed foods, and carbonated beverages is often advised.
Important Considerations:
![]() Hypoparathyroidism is usually a chronic condition that requires lifelong management.
Hypoparathyroidism is usually a chronic condition that requires lifelong management.
![]() Regular monitoring of calcium and phosphorus levels is essential to adjust treatment as needed.
Regular monitoring of calcium and phosphorus levels is essential to adjust treatment as needed.
![]() It is important to see an endocrinologist (a doctor who specializes in hormone disorders) for proper diagnosis and management.
It is important to see an endocrinologist (a doctor who specializes in hormone disorders) for proper diagnosis and management.
![]() Emergency treatment with intravenous calcium may be necessary for severe hypocalcemia.
Emergency treatment with intravenous calcium may be necessary for severe hypocalcemia.
In summary, hypoparathyroidism is a condition characterized by insufficient production of parathyroid hormone, leading to low blood calcium and high blood phosphorus. It can cause a range of symptoms and requires ongoing treatment to maintain normal calcium and phosphorus levels.