Hypothalamic dysfunction, Hypothalamic amenorrhea
Published: 18 Jun 2025
ICD9: 253.9 ICD10: E23.3 ICD11: 5A61.Y
Okay, let's break down "Hypothalamic dysfunction, Hypothalamic amenorrhea.
"
1. Hypothalamus: The Control Center
![]() The hypothalamus is a small but mighty part of the brain located just above the brainstem. It plays a crucial role in regulating many essential bodily functions, including:
The hypothalamus is a small but mighty part of the brain located just above the brainstem. It plays a crucial role in regulating many essential bodily functions, including:![]()

![]() Hormone production: It controls the release of hormones from the pituitary gland (another key endocrine gland).
Hormone production: It controls the release of hormones from the pituitary gland (another key endocrine gland).![]()

![]() Body temperature
Body temperature![]()

![]() Hunger and thirst
Hunger and thirst![]()

![]() Sleep-wake cycles
Sleep-wake cycles![]()

![]() Mood and emotions
Mood and emotions![]()

![]() Reproductive function
Reproductive function
2. Hypothalamic Dysfunction:
![]() Hypothalamic dysfunction simply means that the hypothalamus is not working properly. This can be due to various reasons:
Hypothalamic dysfunction simply means that the hypothalamus is not working properly. This can be due to various reasons:![]()

![]() Stress: Chronic stress (physical or emotional) can disrupt hypothalamic function.
Stress: Chronic stress (physical or emotional) can disrupt hypothalamic function.![]()

![]() Weight loss or being underweight: Insufficient body fat can affect hormone production.
Weight loss or being underweight: Insufficient body fat can affect hormone production.![]()

![]() Excessive exercise: High-intensity or prolonged exercise, especially when combined with low calorie intake, can strain the hypothalamus.
Excessive exercise: High-intensity or prolonged exercise, especially when combined with low calorie intake, can strain the hypothalamus.![]()

![]() Eating disorders: Anorexia nervosa and bulimia are common causes.
Eating disorders: Anorexia nervosa and bulimia are common causes.![]()

![]() Genetic factors: In rare cases, genetic conditions can affect hypothalamic development or function.
Genetic factors: In rare cases, genetic conditions can affect hypothalamic development or function.![]()

![]() Tumors: Tumors in or near the hypothalamus can disrupt its normal activity.
Tumors: Tumors in or near the hypothalamus can disrupt its normal activity.![]()

![]() Infections or inflammation: Infections or inflammatory processes in the brain can sometimes affect the hypothalamus.
Infections or inflammation: Infections or inflammatory processes in the brain can sometimes affect the hypothalamus.![]()

![]() Traumatic brain injury: Injury to the brain can cause damage.
Traumatic brain injury: Injury to the brain can cause damage.
3. Hypothalamic Amenorrhea (HA):
![]() Amenorrhea means the absence of menstruation. There are different types of amenorrhea.
Amenorrhea means the absence of menstruation. There are different types of amenorrhea.
![]() Hypothalamic amenorrhea (HA) specifically refers to the absence of menstruation *due to a problem with the hypothalamus.* It's a type of *secondary amenorrhea* meaning menstruation was once present but has stopped.
Hypothalamic amenorrhea (HA) specifically refers to the absence of menstruation *due to a problem with the hypothalamus.* It's a type of *secondary amenorrhea* meaning menstruation was once present but has stopped.
How it Works (the Chain Reaction):
Here's how hypothalamic dysfunction leads to amenorrhea:
1. Hypothalamus Problems: Something (stress, low weight, etc.) disrupts the hypothalamus's normal function.
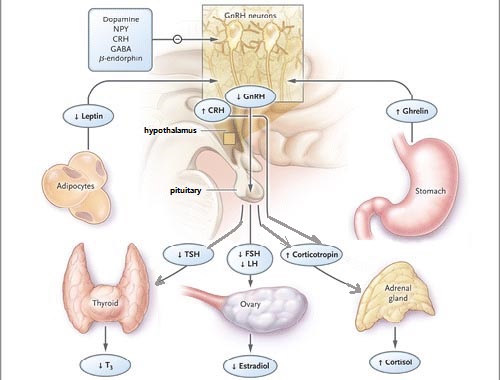
2. GnRH Disruption: The hypothalamus normally releases a hormone called Gonadotropin-Releasing Hormone (GnRH). In HA, GnRH secretion is reduced or becomes erratic (pulsatile).
3. LH and FSH Reduction: GnRH stimulates the pituitary gland to release two more hormones: Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH). Because GnRH is reduced, LH and FSH levels also drop.
4. Ovarian Function Impaired: LH and FSH are essential for the ovaries to function properly. They stimulate the ovaries to produce estrogen and progesterone, which are necessary for ovulation and menstruation. With low LH and FSH, the ovaries don't produce enough estrogen.
5. No Ovulation, No Period: Without sufficient estrogen and normal LH/FSH, ovulation doesn't occur, and the uterine lining doesn't build up and shed as it normally would. This results in the absence of menstruation (amenorrhea).
Key Features of Hypothalamic Amenorrhea:
![]() Absence of periods: Usually for 3 months or more.
Absence of periods: Usually for 3 months or more.
![]() Low estrogen levels: Blood tests will show that estrogen is low.
Low estrogen levels: Blood tests will show that estrogen is low.
![]() Low or normal FSH and LH levels: This helps distinguish HA from other causes of amenorrhea (like Primary Ovarian Insufficiency, where FSH is high).
Low or normal FSH and LH levels: This helps distinguish HA from other causes of amenorrhea (like Primary Ovarian Insufficiency, where FSH is high).
![]() Often associated with:
Often associated with:![]()

![]() Stress
Stress![]()

![]() Weight loss
Weight loss![]()

![]() Excessive exercise
Excessive exercise![]()

![]() Eating disorder history
Eating disorder history
Diagnosis:
A doctor will diagnose hypothalamic amenorrhea by:
![]() Taking a detailed medical history: Including questions about menstrual cycles, weight changes, stress levels, exercise habits, and any underlying medical conditions.
Taking a detailed medical history: Including questions about menstrual cycles, weight changes, stress levels, exercise habits, and any underlying medical conditions.
![]() Performing a physical exam.
Performing a physical exam.
![]() Ordering blood tests: To check hormone levels (estrogen, FSH, LH, prolactin, thyroid hormones), rule out pregnancy, and look for other possible causes of amenorrhea.
Ordering blood tests: To check hormone levels (estrogen, FSH, LH, prolactin, thyroid hormones), rule out pregnancy, and look for other possible causes of amenorrhea.
![]() Ruling out other causes: Pregnancy, thyroid problems, pituitary tumors, and other medical conditions need to be excluded.
Ruling out other causes: Pregnancy, thyroid problems, pituitary tumors, and other medical conditions need to be excluded.
Treatment:
The primary goal of treatment is to address the underlying cause of the hypothalamic dysfunction and restore normal menstrual cycles. Treatment may involve:
![]() Lifestyle modifications:
Lifestyle modifications:![]()

![]() Reducing stress: Stress management techniques (yoga, meditation, therapy) can be helpful.
Reducing stress: Stress management techniques (yoga, meditation, therapy) can be helpful.![]()

![]() Gaining weight (if underweight): Nutritional counseling and a gradual increase in caloric intake are often necessary.
Gaining weight (if underweight): Nutritional counseling and a gradual increase in caloric intake are often necessary.![]()

![]() Modifying exercise habits: Reducing the intensity or frequency of exercise may be needed.
Modifying exercise habits: Reducing the intensity or frequency of exercise may be needed.
![]() Cognitive Behavioral Therapy (CBT): Helpful especially if eating disorders or body image issues are involved.
Cognitive Behavioral Therapy (CBT): Helpful especially if eating disorders or body image issues are involved.
![]() Hormone therapy: Estrogen and progesterone can be prescribed to protect bone health (low estrogen can lead to osteoporosis) and induce a period, but this does not fix the underlying problem.
Hormone therapy: Estrogen and progesterone can be prescribed to protect bone health (low estrogen can lead to osteoporosis) and induce a period, but this does not fix the underlying problem.
![]() Fertility treatment (if desired): If pregnancy is desired, medications to stimulate ovulation may be used. It is often recommended to restore normal cycles first.
Fertility treatment (if desired): If pregnancy is desired, medications to stimulate ovulation may be used. It is often recommended to restore normal cycles first.
Important Considerations:
![]() Bone health: Prolonged low estrogen levels can lead to decreased bone density and an increased risk of osteoporosis.
Bone health: Prolonged low estrogen levels can lead to decreased bone density and an increased risk of osteoporosis.
![]() Fertility: HA can cause infertility because ovulation is not occurring.
Fertility: HA can cause infertility because ovulation is not occurring.
![]() Overall health: It's crucial to address the underlying cause of hypothalamic dysfunction for overall health and well-being.
Overall health: It's crucial to address the underlying cause of hypothalamic dysfunction for overall health and well-being.
In summary, Hypothalamic Amenorrhea is the absence of menstruation due to a problem with the hypothalamus in the brain, usually caused by stress, low weight, or excessive exercise. It is important to seek medical attention to diagnose the condition and address the underlying causes.
![]() Disclaimer: This information is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.*
Disclaimer: This information is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.*