Interstitial cystitis (Bladder pain syndrome)
Published: 18 Jun 2025
ICD9: 595.1 ICD10: N30.10 ICD11: GC00.3
Interstitial cystitis (IC), also known as bladder pain syndrome (BPS), is a chronic condition causing bladder pressure, bladder pain, and sometimes pelvic pain.
The pain ranges from mild discomfort to severe. The bladder is a muscular organ that stores urine. When you urinate, nerves signal your bladder to release urine. With IC/BPS, these signals get mixed up — you feel the need to urinate more often and with smaller volumes of urine than most people.
Here's a breakdown of key aspects of IC/BPS:
Symptoms:
![]() Pain in the pelvis or between the vagina and anus in women, and between the scrotum and anus in men: This is a hallmark symptom and can be constant or intermittent.
Pain in the pelvis or between the vagina and anus in women, and between the scrotum and anus in men: This is a hallmark symptom and can be constant or intermittent.
![]() Chronic pelvic pain: The pain can extend beyond the bladder and affect the lower abdomen, back, and thighs.
Chronic pelvic pain: The pain can extend beyond the bladder and affect the lower abdomen, back, and thighs.
![]() Persistent, frequent urge to urinate: The urge can be very strong and difficult to ignore.
Persistent, frequent urge to urinate: The urge can be very strong and difficult to ignore.
![]() Frequent urination, often of small amounts, throughout the day and night (nocturia): People with IC/BPS may urinate many times a day (more than 8-10 times in 24 hours is common) and frequently get up to urinate during the night.
Frequent urination, often of small amounts, throughout the day and night (nocturia): People with IC/BPS may urinate many times a day (more than 8-10 times in 24 hours is common) and frequently get up to urinate during the night.
![]() Pain or discomfort while the bladder fills: The pain typically increases as the bladder fills and decreases after urination.
Pain or discomfort while the bladder fills: The pain typically increases as the bladder fills and decreases after urination.
![]() Pain during sexual intercourse: This is common, especially in women.
Pain during sexual intercourse: This is common, especially in women.
Other Symptoms:
![]() Burning sensation during urination (though this is often associated with urinary tract infection, it can occur in IC/BPS without infection)
Burning sensation during urination (though this is often associated with urinary tract infection, it can occur in IC/BPS without infection)
![]() Pain relief after urination (temporary)
Pain relief after urination (temporary)
Causes:
The exact cause of IC/BPS is not fully understood. Several factors may contribute to the condition, including:
![]() Defect in the bladder lining (epithelium): A "leaky" bladder lining may allow irritating substances in the urine to penetrate the bladder wall, causing inflammation and pain.
Defect in the bladder lining (epithelium): A "leaky" bladder lining may allow irritating substances in the urine to penetrate the bladder wall, causing inflammation and pain.
![]() Mast cell activation: Mast cells are part of the immune system. They release histamine and other chemicals that can cause inflammation.
Mast cell activation: Mast cells are part of the immune system. They release histamine and other chemicals that can cause inflammation.
![]() Nerve abnormalities: Increased sensitivity or abnormal nerve function in the bladder can lead to pain signals being misinterpreted.
Nerve abnormalities: Increased sensitivity or abnormal nerve function in the bladder can lead to pain signals being misinterpreted.
![]() Autoimmune reaction: The body's immune system may attack the bladder.
Autoimmune reaction: The body's immune system may attack the bladder.
![]() Genetic factors: There may be a genetic predisposition to developing IC/BPS.
Genetic factors: There may be a genetic predisposition to developing IC/BPS.
![]() Infection: While IC/BPS is NOT a bladder infection, a previous infection might trigger the condition in some people.
Infection: While IC/BPS is NOT a bladder infection, a previous infection might trigger the condition in some people.
Diagnosis:
Diagnosing IC/BPS can be challenging, as there is no single definitive test. Diagnosis is usually based on a combination of factors:
![]() Medical history: The doctor will ask about your symptoms, medical history, and any other relevant information.
Medical history: The doctor will ask about your symptoms, medical history, and any other relevant information.
![]() Physical exam: The doctor will perform a physical examination, including a pelvic exam (in women).
Physical exam: The doctor will perform a physical examination, including a pelvic exam (in women).
![]() Urine analysis: This test rules out a urinary tract infection (UTI). Crucially, IC/BPS is *not* a UTI and will not be treated by antibiotics.
Urine analysis: This test rules out a urinary tract infection (UTI). Crucially, IC/BPS is *not* a UTI and will not be treated by antibiotics.
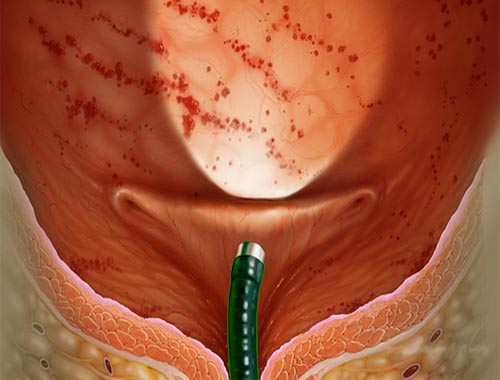
![]() Cystoscopy: This procedure involves inserting a thin, flexible tube with a camera (cystoscope) into the bladder to examine the bladder lining. Hydrodistension (stretching the bladder) is often performed during cystoscopy. This can sometimes provide temporary relief but can also temporarily worsen symptoms. Findings can include inflammation, ulcers (Hunner's lesions), and pinpoint bleeding. However, many people with IC/BPS have normal-appearing bladders during cystoscopy.
Cystoscopy: This procedure involves inserting a thin, flexible tube with a camera (cystoscope) into the bladder to examine the bladder lining. Hydrodistension (stretching the bladder) is often performed during cystoscopy. This can sometimes provide temporary relief but can also temporarily worsen symptoms. Findings can include inflammation, ulcers (Hunner's lesions), and pinpoint bleeding. However, many people with IC/BPS have normal-appearing bladders during cystoscopy.
![]() Biopsy: A bladder biopsy may be taken during cystoscopy to rule out other conditions, such as bladder cancer.
Biopsy: A bladder biopsy may be taken during cystoscopy to rule out other conditions, such as bladder cancer.
![]() Potassium sensitivity test: This test involves instilling potassium chloride into the bladder to see if it provokes pain. People with IC/BPS are often more sensitive to potassium.
Potassium sensitivity test: This test involves instilling potassium chloride into the bladder to see if it provokes pain. People with IC/BPS are often more sensitive to potassium.
![]() Voiding diary: This involves recording how frequently you urinate and the volume of urine each time.
Voiding diary: This involves recording how frequently you urinate and the volume of urine each time.
Treatment:
There is no cure for IC/BPS, and treatment focuses on managing symptoms and improving quality of life. Treatment approaches often involve a combination of therapies:
![]() Lifestyle changes:
Lifestyle changes:![]()

![]() Dietary modifications: Identifying and avoiding trigger foods and beverages. Common triggers include caffeine, alcohol, citrus fruits, spicy foods, carbonated drinks, and artificial sweeteners.
Dietary modifications: Identifying and avoiding trigger foods and beverages. Common triggers include caffeine, alcohol, citrus fruits, spicy foods, carbonated drinks, and artificial sweeteners.![]()

![]() Fluid management: Drinking adequate fluids, but avoiding excessive fluid intake before bedtime.
Fluid management: Drinking adequate fluids, but avoiding excessive fluid intake before bedtime.![]()

![]() Bladder training: Learning to control the urge to urinate and gradually increasing the time between voiding.
Bladder training: Learning to control the urge to urinate and gradually increasing the time between voiding.![]()

![]() Stress management: Using relaxation techniques, such as meditation or yoga, to reduce stress.
Stress management: Using relaxation techniques, such as meditation or yoga, to reduce stress.
![]() Medications:
Medications:![]()

![]() Oral Medications:
Oral Medications:![]()

![]() Pentosan polysulfate sodium (Elmiron): This medication is thought to help repair the bladder lining. (There are concerns about long-term use and potential vision problems, so discuss this with your doctor.)
Pentosan polysulfate sodium (Elmiron): This medication is thought to help repair the bladder lining. (There are concerns about long-term use and potential vision problems, so discuss this with your doctor.)![]()

![]() Antihistamines: These can help reduce inflammation and relieve urinary frequency and urgency. (e.g., hydroxyzine)
Antihistamines: These can help reduce inflammation and relieve urinary frequency and urgency. (e.g., hydroxyzine)![]()

![]() Tricyclic antidepressants: These can help reduce pain and improve sleep. (e.g., amitriptyline)
Tricyclic antidepressants: These can help reduce pain and improve sleep. (e.g., amitriptyline)![]()

![]() Pain relievers: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, may help with mild pain. In some cases, stronger pain medications may be prescribed.
Pain relievers: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, may help with mild pain. In some cases, stronger pain medications may be prescribed.![]()

![]() Bladder Instillations:
Bladder Instillations:![]()

![]() Dimethyl sulfoxide (DMSO): This medication is instilled directly into the bladder and is thought to reduce inflammation and pain.
Dimethyl sulfoxide (DMSO): This medication is instilled directly into the bladder and is thought to reduce inflammation and pain.![]()

![]() Lidocaine and bicarbonate: These are sometimes used in combination as bladder instillations to provide pain relief.
Lidocaine and bicarbonate: These are sometimes used in combination as bladder instillations to provide pain relief.![]()

![]() Heparin: This can help to protect the bladder lining.
Heparin: This can help to protect the bladder lining.
![]() Physical Therapy: Pelvic floor physical therapy can help strengthen and relax the pelvic floor muscles, which can reduce pain and improve bladder control.
Physical Therapy: Pelvic floor physical therapy can help strengthen and relax the pelvic floor muscles, which can reduce pain and improve bladder control.
![]() Bladder Distention: Stretching the bladder with fluid can sometimes provide temporary symptom relief.
Bladder Distention: Stretching the bladder with fluid can sometimes provide temporary symptom relief.
![]() Nerve Stimulation:
Nerve Stimulation:![]()

![]() Transcutaneous electrical nerve stimulation (TENS): This involves using a mild electrical current to stimulate nerves and reduce pain.
Transcutaneous electrical nerve stimulation (TENS): This involves using a mild electrical current to stimulate nerves and reduce pain.![]()

![]() Sacral nerve stimulation (InterStim): This involves implanting a device that stimulates the sacral nerves, which control bladder function.
Sacral nerve stimulation (InterStim): This involves implanting a device that stimulates the sacral nerves, which control bladder function.![]()

![]() Percutaneous tibial nerve stimulation (PTNS): This involves stimulating the tibial nerve in the ankle, which can help improve bladder control.
Percutaneous tibial nerve stimulation (PTNS): This involves stimulating the tibial nerve in the ankle, which can help improve bladder control.
![]() Surgery: Surgery is rarely used for IC/BPS, and it is typically considered only as a last resort when other treatments have failed. Surgical options include bladder augmentation (enlarging the bladder) and urinary diversion (creating a new way for urine to exit the body). However, surgery is NOT guaranteed to relieve symptoms and can sometimes worsen them.
Surgery: Surgery is rarely used for IC/BPS, and it is typically considered only as a last resort when other treatments have failed. Surgical options include bladder augmentation (enlarging the bladder) and urinary diversion (creating a new way for urine to exit the body). However, surgery is NOT guaranteed to relieve symptoms and can sometimes worsen them.
![]() Complementary and Alternative Therapies:
Complementary and Alternative Therapies:![]()

![]() Acupuncture
Acupuncture![]()

![]() Herbal remedies (consult with a healthcare professional before using any herbal remedies)
Herbal remedies (consult with a healthcare professional before using any herbal remedies)![]()

![]() Biofeedback
Biofeedback
Important Considerations:
![]() Individualized Treatment: Treatment for IC/BPS is highly individualized. What works for one person may not work for another. It often takes time and experimentation to find the most effective treatment plan.
Individualized Treatment: Treatment for IC/BPS is highly individualized. What works for one person may not work for another. It often takes time and experimentation to find the most effective treatment plan.
![]() Psychological Support: Living with chronic pain can be difficult and can lead to anxiety, depression, and other mental health issues. Psychological support, such as therapy or support groups, can be very helpful.
Psychological Support: Living with chronic pain can be difficult and can lead to anxiety, depression, and other mental health issues. Psychological support, such as therapy or support groups, can be very helpful.
![]() Finding a Specialist: It's important to find a doctor who is knowledgeable about IC/BPS and experienced in treating the condition. Urologists (doctors specializing in the urinary tract) are often the primary care providers for IC/BPS, but gynecologists, pain specialists, and other healthcare professionals may also be involved in your care.
Finding a Specialist: It's important to find a doctor who is knowledgeable about IC/BPS and experienced in treating the condition. Urologists (doctors specializing in the urinary tract) are often the primary care providers for IC/BPS, but gynecologists, pain specialists, and other healthcare professionals may also be involved in your care.
![]() Long-Term Condition: IC/BPS is a chronic condition, meaning that it is long-lasting. There may be periods of remission (when symptoms are mild or absent) and flares (when symptoms worsen). It's important to work with your doctor to develop a long-term management plan.
Long-Term Condition: IC/BPS is a chronic condition, meaning that it is long-lasting. There may be periods of remission (when symptoms are mild or absent) and flares (when symptoms worsen). It's important to work with your doctor to develop a long-term management plan.
![]() Research: Research into IC/BPS is ongoing, and new treatments are being developed all the time. Staying informed about the latest research can help you make informed decisions about your care.
Research: Research into IC/BPS is ongoing, and new treatments are being developed all the time. Staying informed about the latest research can help you make informed decisions about your care.
In summary, interstitial cystitis/bladder pain syndrome is a complex and often debilitating condition characterized by bladder pain, urinary frequency, and urgency. Diagnosis can be challenging, and treatment is aimed at managing symptoms and improving quality of life.