Irritable bowel syndrome (IBS)
Published: 18 Jun 2025
ICD9: 564.1 ICD10: K58.9 ICD11: DD91
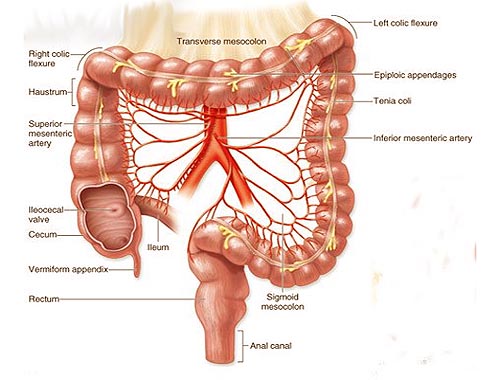
Irritable Bowel Syndrome (IBS) is a common disorder that affects the large intestine.
It's a chronic condition, meaning it's long-lasting, and while it can cause significant discomfort, it doesn't damage the intestines or increase the risk of colon cancer.
Key Characteristics of IBS:
![]() Abdominal Pain: This is a hallmark symptom. The pain is often related to bowel movements and can be relieved or worsened after going to the bathroom.
Abdominal Pain: This is a hallmark symptom. The pain is often related to bowel movements and can be relieved or worsened after going to the bathroom.
![]() Changes in Bowel Habits: IBS is characterized by altered bowel habits, which can include:
Changes in Bowel Habits: IBS is characterized by altered bowel habits, which can include:![]()

![]() Diarrhea (IBS-D): Frequent, loose, and watery stools.
Diarrhea (IBS-D): Frequent, loose, and watery stools.![]()

![]() Constipation (IBS-C): Difficulty passing stools, infrequent bowel movements, and hard stools.
Constipation (IBS-C): Difficulty passing stools, infrequent bowel movements, and hard stools.![]()

![]() Mixed (IBS-M): Alternating between diarrhea and constipation.
Mixed (IBS-M): Alternating between diarrhea and constipation.
![]() Bloating and Gas: Many people with IBS experience excessive bloating and gas.
Bloating and Gas: Many people with IBS experience excessive bloating and gas.
Symptoms of IBS:
The symptoms of IBS can vary widely from person to person and can fluctuate in intensity. Common symptoms include:
![]() Abdominal pain or cramping
Abdominal pain or cramping
![]() Bloating
Bloating
![]() Gas
Gas
![]() Diarrhea or constipation, or alternating between the two
Diarrhea or constipation, or alternating between the two
![]() Mucus in the stool
Mucus in the stool
![]() Feeling like you haven't completely emptied your bowels after a bowel movement
Feeling like you haven't completely emptied your bowels after a bowel movement
![]() Urgent need to have a bowel movement
Urgent need to have a bowel movement
What Causes IBS?
The exact cause of IBS is not fully understood, but it's believed to be a combination of factors, including:
![]() Gut Motility Problems: Abnormal contractions of the muscles in the intestines can lead to diarrhea or constipation.
Gut Motility Problems: Abnormal contractions of the muscles in the intestines can lead to diarrhea or constipation.
![]() Visceral Hypersensitivity: People with IBS may have a lower pain threshold in the gut, making them more sensitive to normal gut sensations.
Visceral Hypersensitivity: People with IBS may have a lower pain threshold in the gut, making them more sensitive to normal gut sensations.
![]() Brain-Gut Connection: The brain and gut are closely connected. Stress, anxiety, and depression can trigger or worsen IBS symptoms.
Brain-Gut Connection: The brain and gut are closely connected. Stress, anxiety, and depression can trigger or worsen IBS symptoms.
![]() Gut Microbiome Imbalances: Changes in the balance of bacteria in the gut may contribute to IBS.
Gut Microbiome Imbalances: Changes in the balance of bacteria in the gut may contribute to IBS.
![]() Post-Infectious IBS: Some people develop IBS after a bout of gastroenteritis (a stomach bug).
Post-Infectious IBS: Some people develop IBS after a bout of gastroenteritis (a stomach bug).
![]() Food Sensitivities/Intolerances: Certain foods can trigger IBS symptoms in some individuals. Common culprits include:
Food Sensitivities/Intolerances: Certain foods can trigger IBS symptoms in some individuals. Common culprits include:![]()

![]() Dairy products
Dairy products![]()

![]() Gluten (found in wheat, barley, and rye)
Gluten (found in wheat, barley, and rye)![]()

![]() Certain fruits and vegetables
Certain fruits and vegetables![]()

![]() Artificial sweeteners
Artificial sweeteners![]()

![]() Carbonated beverages
Carbonated beverages![]()

![]() High-FODMAP foods (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols)
High-FODMAP foods (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols)
Diagnosis:
There is no specific test to diagnose IBS. Diagnosis is typically based on a medical history, a physical exam, and ruling out other conditions. Doctors may use the Rome criteria (a set of standardized symptom criteria) to help diagnose IBS. They might also order tests such as:
![]() Stool tests: To check for infection or inflammation.
Stool tests: To check for infection or inflammation.
![]() Blood tests: To rule out other conditions like celiac disease or inflammatory bowel disease (IBD).
Blood tests: To rule out other conditions like celiac disease or inflammatory bowel disease (IBD).
![]() Colonoscopy: To visualize the colon and rule out more serious problems, especially if there are alarming symptoms like bleeding or unexplained weight loss.
Colonoscopy: To visualize the colon and rule out more serious problems, especially if there are alarming symptoms like bleeding or unexplained weight loss.
![]() Flexible Sigmoidoscopy: Similar to colonoscopy, but examines only the lower part of the colon.
Flexible Sigmoidoscopy: Similar to colonoscopy, but examines only the lower part of the colon.
![]() Lactose intolerance test: To check for lactose intolerance.
Lactose intolerance test: To check for lactose intolerance.
Treatment:
There is no cure for IBS, but symptoms can be managed with lifestyle changes, diet modifications, and medications. Treatment is tailored to the individual's specific symptoms.
![]() Lifestyle Changes:
Lifestyle Changes:![]()

![]() Stress Management: Techniques like meditation, yoga, deep breathing exercises, and regular exercise can help reduce stress.
Stress Management: Techniques like meditation, yoga, deep breathing exercises, and regular exercise can help reduce stress.![]()

![]() Regular Exercise: Physical activity can help regulate bowel function.
Regular Exercise: Physical activity can help regulate bowel function.![]()

![]() Adequate Sleep: Getting enough sleep can help improve overall health and reduce stress.
Adequate Sleep: Getting enough sleep can help improve overall health and reduce stress.
![]() Dietary Changes:
Dietary Changes:![]()

![]() Identifying Trigger Foods: Keeping a food diary can help identify foods that trigger symptoms.
Identifying Trigger Foods: Keeping a food diary can help identify foods that trigger symptoms.![]()

![]() The Low-FODMAP Diet: This diet involves restricting certain types of carbohydrates that are poorly absorbed in the small intestine and can contribute to gas, bloating, and diarrhea. It is typically implemented under the guidance of a registered dietitian.
The Low-FODMAP Diet: This diet involves restricting certain types of carbohydrates that are poorly absorbed in the small intestine and can contribute to gas, bloating, and diarrhea. It is typically implemented under the guidance of a registered dietitian.![]()

![]() Increasing Fiber Intake: Fiber can help regulate bowel movements, but it's important to increase fiber gradually to avoid worsening symptoms. Soluble fiber may be better tolerated than insoluble fiber.
Increasing Fiber Intake: Fiber can help regulate bowel movements, but it's important to increase fiber gradually to avoid worsening symptoms. Soluble fiber may be better tolerated than insoluble fiber.![]()

![]() Staying Hydrated: Drinking plenty of water can help prevent constipation.
Staying Hydrated: Drinking plenty of water can help prevent constipation.![]()

![]() Eating Regular Meals: Skipping meals can disrupt bowel function.
Eating Regular Meals: Skipping meals can disrupt bowel function.
![]() Medications:
Medications:![]()

![]() Antidiarrheals: Such as loperamide (Imodium) can help reduce diarrhea.
Antidiarrheals: Such as loperamide (Imodium) can help reduce diarrhea.![]()

![]() Laxatives: Can help relieve constipation.
Laxatives: Can help relieve constipation.![]()

![]() Antispasmodics: Such as dicyclomine (Bentyl) can help reduce abdominal cramping.
Antispasmodics: Such as dicyclomine (Bentyl) can help reduce abdominal cramping.![]()

![]() Antidepressants: Low doses of certain antidepressants can help reduce pain and improve bowel function.
Antidepressants: Low doses of certain antidepressants can help reduce pain and improve bowel function.![]()

![]() Probiotics: May help restore a healthy balance of gut bacteria. The effectiveness of specific strains of probiotics can vary.
Probiotics: May help restore a healthy balance of gut bacteria. The effectiveness of specific strains of probiotics can vary.![]()

![]() Other Medications: Several newer medications are available for specific types of IBS, such as those with diarrhea or constipation as the primary symptom. Examples include:
Other Medications: Several newer medications are available for specific types of IBS, such as those with diarrhea or constipation as the primary symptom. Examples include:![]()

![]() Lubiprostone (Amitiza): For IBS-C
Lubiprostone (Amitiza): For IBS-C![]()

![]() Linaclotide (Linzess): For IBS-C
Linaclotide (Linzess): For IBS-C![]()

![]() Eluxadoline (Viberzi): For IBS-D
Eluxadoline (Viberzi): For IBS-D![]()

![]() Rifaximin (Xifaxan): An antibiotic that can help reduce diarrhea.
Rifaximin (Xifaxan): An antibiotic that can help reduce diarrhea.
When to See a Doctor:
It's important to see a doctor if you have persistent changes in bowel habits, abdominal pain, or other symptoms that are concerning. Seek medical attention right away if you experience:
![]() Rectal bleeding
Rectal bleeding
![]() Unexplained weight loss
Unexplained weight loss
![]() Persistent diarrhea or constipation that doesn't respond to over-the-counter treatments
Persistent diarrhea or constipation that doesn't respond to over-the-counter treatments
![]() Severe abdominal pain
Severe abdominal pain
![]() Anemia symptoms (fatigue, weakness)
Anemia symptoms (fatigue, weakness)
Living with IBS:
IBS can significantly impact a person's quality of life. However, with proper management, many people can successfully control their symptoms and live full and active lives. It's important to work closely with your doctor to develop a treatment plan that's right for you. Support groups and online communities can also be helpful for people with IBS.