Myelofibrosis
Published: 18 Jun 2025
ICD9: 289.83 ICD10: D75.81 ICD11: 2A20.2
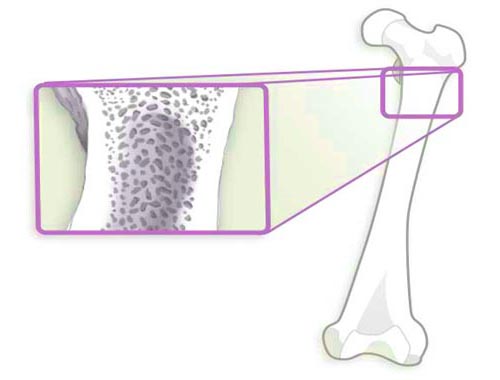
Myelofibrosis is a rare type of bone marrow cancer that disrupts the body's normal production of blood cells.
It results in extensive scarring in the bone marrow, leading to severe anemia, weakness, fatigue, and often an enlarged spleen.
Here's a breakdown of key aspects:
What Happens in Myelofibrosis:
![]() Normal Bone Marrow Function: Healthy bone marrow contains stem cells that develop into red blood cells (carry oxygen), white blood cells (fight infection), and platelets (help with blood clotting).
Normal Bone Marrow Function: Healthy bone marrow contains stem cells that develop into red blood cells (carry oxygen), white blood cells (fight infection), and platelets (help with blood clotting).
![]() Fibrosis (Scarring): In myelofibrosis, the bone marrow becomes increasingly scarred (fibrotic) due to an overproduction of abnormal cells, specifically megakaryocytes (cells that produce platelets). This scarring crowds out the normal blood-forming cells.
Fibrosis (Scarring): In myelofibrosis, the bone marrow becomes increasingly scarred (fibrotic) due to an overproduction of abnormal cells, specifically megakaryocytes (cells that produce platelets). This scarring crowds out the normal blood-forming cells.
![]() Ineffective Blood Cell Production: The scarred bone marrow struggles to produce enough healthy blood cells.
Ineffective Blood Cell Production: The scarred bone marrow struggles to produce enough healthy blood cells.
![]() Extramedullary Hematopoiesis: Because the bone marrow is failing, the body tries to compensate by producing blood cells in other organs, primarily the spleen and liver. This can lead to significant enlargement of these organs.
Extramedullary Hematopoiesis: Because the bone marrow is failing, the body tries to compensate by producing blood cells in other organs, primarily the spleen and liver. This can lead to significant enlargement of these organs.
Key Characteristics and Consequences:
![]() Anemia: Lack of red blood cells, causing fatigue, weakness, and shortness of breath. This is often a primary symptom.
Anemia: Lack of red blood cells, causing fatigue, weakness, and shortness of breath. This is often a primary symptom.
![]() Thrombocytopenia: Low platelet count, increasing the risk of bleeding and bruising.
Thrombocytopenia: Low platelet count, increasing the risk of bleeding and bruising.
![]() Leukopenia (or Leukocytosis): Low or high white blood cell count, which can increase the risk of infection. The count is often abnormal.
Leukopenia (or Leukocytosis): Low or high white blood cell count, which can increase the risk of infection. The count is often abnormal.
![]() Splenomegaly: Enlarged spleen, causing abdominal discomfort, pain, and early satiety (feeling full quickly). The enlarged spleen can also contribute to anemia and thrombocytopenia.
Splenomegaly: Enlarged spleen, causing abdominal discomfort, pain, and early satiety (feeling full quickly). The enlarged spleen can also contribute to anemia and thrombocytopenia.
![]() Symptoms: Common symptoms include:
Symptoms: Common symptoms include:![]()

![]() Fatigue
Fatigue![]()

![]() Shortness of breath
Shortness of breath![]()

![]() Weakness
Weakness![]()

![]() Bone pain
Bone pain![]()

![]() Easy bleeding and bruising
Easy bleeding and bruising![]()

![]() Night sweats
Night sweats![]()

![]() Fever
Fever![]()

![]() Weight loss
Weight loss![]()

![]() Abdominal pain or fullness due to enlarged spleen
Abdominal pain or fullness due to enlarged spleen
![]() Progressive Disease: Myelofibrosis is generally a progressive disease, meaning it worsens over time.
Progressive Disease: Myelofibrosis is generally a progressive disease, meaning it worsens over time.
Types of Myelofibrosis:
![]() Primary Myelofibrosis (PMF): This is the most common type, occurring on its own, without a known preceding bone marrow disorder.
Primary Myelofibrosis (PMF): This is the most common type, occurring on its own, without a known preceding bone marrow disorder.
![]() Secondary Myelofibrosis (Post-Polycythemia Vera Myelofibrosis or Post-Essential Thrombocythemia Myelofibrosis): This type develops as a complication of other bone marrow disorders, namely polycythemia vera (PV) or essential thrombocythemia (ET).
Secondary Myelofibrosis (Post-Polycythemia Vera Myelofibrosis or Post-Essential Thrombocythemia Myelofibrosis): This type develops as a complication of other bone marrow disorders, namely polycythemia vera (PV) or essential thrombocythemia (ET).
Causes and Risk Factors:
![]() Genetic Mutations: Most cases of myelofibrosis are linked to genetic mutations, particularly in genes like *JAK2*, *CALR*, and *MPL*. These mutations are usually acquired during a person's lifetime and are not inherited.
Genetic Mutations: Most cases of myelofibrosis are linked to genetic mutations, particularly in genes like *JAK2*, *CALR*, and *MPL*. These mutations are usually acquired during a person's lifetime and are not inherited.
![]() Exposure to Certain Chemicals: Prolonged exposure to industrial chemicals like benzene and toluene may increase the risk.
Exposure to Certain Chemicals: Prolonged exposure to industrial chemicals like benzene and toluene may increase the risk.
![]() Radiation Exposure: High doses of radiation can increase the risk.
Radiation Exposure: High doses of radiation can increase the risk.
![]() Age: The risk of developing myelofibrosis increases with age.
Age: The risk of developing myelofibrosis increases with age.
![]() Prior treatment for cancer: Some cancer treatments, especially chemotherapy and radiation, can increase the risk of developing myelofibrosis later in life.
Prior treatment for cancer: Some cancer treatments, especially chemotherapy and radiation, can increase the risk of developing myelofibrosis later in life.
Diagnosis:
![]() Blood Tests: Complete blood count (CBC) to assess red blood cell, white blood cell, and platelet levels.
Blood Tests: Complete blood count (CBC) to assess red blood cell, white blood cell, and platelet levels.
![]() Bone Marrow Biopsy and Aspiration: Essential for diagnosis. A sample of bone marrow is examined under a microscope to look for scarring and abnormal cells. Genetic testing is often performed on the bone marrow sample.
Bone Marrow Biopsy and Aspiration: Essential for diagnosis. A sample of bone marrow is examined under a microscope to look for scarring and abnormal cells. Genetic testing is often performed on the bone marrow sample.
![]() Physical Examination: To check for enlarged spleen and liver.
Physical Examination: To check for enlarged spleen and liver.
![]() Genetic Testing: To identify specific gene mutations that may be driving the disease.
Genetic Testing: To identify specific gene mutations that may be driving the disease.
![]() Imaging Studies: Ultrasound or CT scans may be used to assess the size of the spleen and liver.
Imaging Studies: Ultrasound or CT scans may be used to assess the size of the spleen and liver.
Treatment:
Treatment for myelofibrosis is aimed at managing symptoms and slowing the progression of the disease. Options include:
![]() Medications:
Medications:![]()

![]() JAK inhibitors (e.g., ruxolitinib, fedratinib): These drugs target the *JAK2* mutation and can help reduce spleen size and improve symptoms like fatigue, night sweats, and bone pain.
JAK inhibitors (e.g., ruxolitinib, fedratinib): These drugs target the *JAK2* mutation and can help reduce spleen size and improve symptoms like fatigue, night sweats, and bone pain.![]()

![]() Danazol: A synthetic androgen that can sometimes improve red blood cell counts.
Danazol: A synthetic androgen that can sometimes improve red blood cell counts.![]()

![]() Thalidomide or lenalidomide: Immunomodulatory drugs that may help reduce spleen size and improve blood counts in some patients.
Thalidomide or lenalidomide: Immunomodulatory drugs that may help reduce spleen size and improve blood counts in some patients.![]()

![]() Hydroxyurea: A chemotherapy drug that can help lower white blood cell and platelet counts.
Hydroxyurea: A chemotherapy drug that can help lower white blood cell and platelet counts.
![]() Blood Transfusions: To treat anemia.
Blood Transfusions: To treat anemia.
![]() Splenectomy (Surgical Removal of the Spleen): May be considered if the enlarged spleen is causing significant problems and medications are not effective.
Splenectomy (Surgical Removal of the Spleen): May be considered if the enlarged spleen is causing significant problems and medications are not effective.
![]() Radiation Therapy: May be used to shrink the spleen or to treat bone pain.
Radiation Therapy: May be used to shrink the spleen or to treat bone pain.
![]() Stem Cell Transplant (Bone Marrow Transplant): The only potentially curative treatment for myelofibrosis. It involves replacing the patient's abnormal bone marrow with healthy stem cells from a donor. However, it is a high-risk procedure and is typically reserved for younger, otherwise healthy patients with high-risk disease.
Stem Cell Transplant (Bone Marrow Transplant): The only potentially curative treatment for myelofibrosis. It involves replacing the patient's abnormal bone marrow with healthy stem cells from a donor. However, it is a high-risk procedure and is typically reserved for younger, otherwise healthy patients with high-risk disease.
![]() Clinical Trials: Investigational therapies may be available through clinical trials.
Clinical Trials: Investigational therapies may be available through clinical trials.
Prognosis:
The prognosis for myelofibrosis varies depending on several factors, including age, the presence of certain genetic mutations, blood counts, and the severity of symptoms. Scoring systems, such as the International Prognostic Scoring System (IPSS) and the Dynamic IPSS (DIPSS), are used to estimate the risk of disease progression and survival.
Important Considerations:
![]() Consultation with a Hematologist: If you suspect you may have myelofibrosis, it's crucial to see a hematologist (a doctor who specializes in blood disorders) for diagnosis and treatment.
Consultation with a Hematologist: If you suspect you may have myelofibrosis, it's crucial to see a hematologist (a doctor who specializes in blood disorders) for diagnosis and treatment.
![]() Individualized Treatment: Treatment plans are tailored to each individual's specific needs and disease characteristics.
Individualized Treatment: Treatment plans are tailored to each individual's specific needs and disease characteristics.
![]() Ongoing Monitoring: Regular monitoring of blood counts and other parameters is important to assess treatment response and detect any complications.
Ongoing Monitoring: Regular monitoring of blood counts and other parameters is important to assess treatment response and detect any complications.
In summary, myelofibrosis is a serious bone marrow disorder that requires careful management by a hematologist. While there is no cure for most patients besides stem cell transplant, treatments are available to manage symptoms and improve quality of life.