Myocarditis
Published: 18 Jun 2025
ICD9: 422 ICD10: I51.4 ICD11: BC42
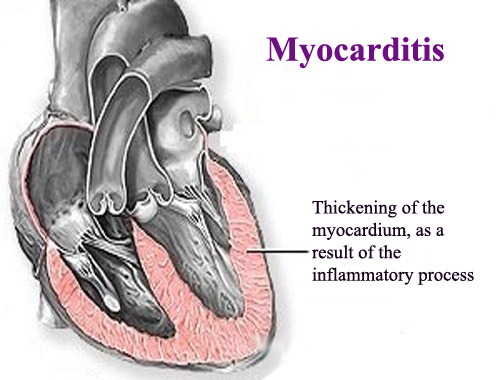
Myocarditis is inflammation of the heart muscle (myocardium).
This inflammation can weaken the heart, making it harder to pump blood throughout the body.
Here's a more detailed breakdown:
![]() What it affects: Primarily the heart muscle (myocardium), but it can sometimes involve the heart's electrical system, causing arrhythmias (irregular heartbeats). It can also lead to pericarditis (inflammation of the sac surrounding the heart) in some cases, termed myopericarditis.
What it affects: Primarily the heart muscle (myocardium), but it can sometimes involve the heart's electrical system, causing arrhythmias (irregular heartbeats). It can also lead to pericarditis (inflammation of the sac surrounding the heart) in some cases, termed myopericarditis.
![]() Causes:
Causes:![]()

![]() Viral Infections: This is the most common cause. Viruses like adenovirus, coxsackievirus, parvovirus B19, and others can directly infect the heart or trigger an immune response that damages it. COVID-19 and its mRNA vaccines have been linked to myocarditis, particularly in young males, although the risk is generally considered low.
Viral Infections: This is the most common cause. Viruses like adenovirus, coxsackievirus, parvovirus B19, and others can directly infect the heart or trigger an immune response that damages it. COVID-19 and its mRNA vaccines have been linked to myocarditis, particularly in young males, although the risk is generally considered low.![]()

![]() Bacterial Infections: Less common than viral causes, but bacteria like streptococcus (which can lead to rheumatic fever) or Lyme disease can cause myocarditis.
Bacterial Infections: Less common than viral causes, but bacteria like streptococcus (which can lead to rheumatic fever) or Lyme disease can cause myocarditis.![]()

![]() Fungal Infections: Fungi can cause myocarditis, especially in people with weakened immune systems.
Fungal Infections: Fungi can cause myocarditis, especially in people with weakened immune systems.![]()

![]() Parasitic Infections: Certain parasites, such as those that cause Chagas disease or toxoplasmosis, can infect the heart.
Parasitic Infections: Certain parasites, such as those that cause Chagas disease or toxoplasmosis, can infect the heart.![]()

![]() Autoimmune Diseases: Conditions like lupus, rheumatoid arthritis, and sarcoidosis can cause inflammation in the heart.
Autoimmune Diseases: Conditions like lupus, rheumatoid arthritis, and sarcoidosis can cause inflammation in the heart.![]()

![]() Medications: Some drugs (prescription and illicit) can lead to myocarditis as a side effect.
Medications: Some drugs (prescription and illicit) can lead to myocarditis as a side effect.![]()

![]() Exposure to Toxins: Certain chemicals and toxins can damage the heart muscle.
Exposure to Toxins: Certain chemicals and toxins can damage the heart muscle.![]()

![]() Idiopathic: In some cases, the cause is unknown (idiopathic myocarditis).
Idiopathic: In some cases, the cause is unknown (idiopathic myocarditis).
![]() Symptoms: Symptoms can vary widely, from mild and unnoticeable to severe and life-threatening. Common symptoms include:
Symptoms: Symptoms can vary widely, from mild and unnoticeable to severe and life-threatening. Common symptoms include:![]()

![]() Chest pain
Chest pain![]()

![]() Fatigue
Fatigue![]()

![]() Shortness of breath (especially during exercise or lying down)
Shortness of breath (especially during exercise or lying down)![]()

![]() Heart palpitations or arrhythmias (irregular heartbeats)
Heart palpitations or arrhythmias (irregular heartbeats)![]()

![]() Swelling in the legs, ankles, and feet (edema)
Swelling in the legs, ankles, and feet (edema)![]()

![]() Dizziness or lightheadedness
Dizziness or lightheadedness![]()

![]() Fainting
Fainting![]()

![]() Sudden cardiac arrest (in severe cases)
Sudden cardiac arrest (in severe cases)![]()

![]() Fever, headache, muscle aches (especially if related to a viral infection)
Fever, headache, muscle aches (especially if related to a viral infection)![]()

![]() Infants may have feeding problems, irritability, and poor growth.
Infants may have feeding problems, irritability, and poor growth.
![]() Diagnosis:
Diagnosis:![]()

![]() Physical Exam: Listening to the heart and lungs, checking for signs of fluid retention.
Physical Exam: Listening to the heart and lungs, checking for signs of fluid retention.![]()

![]() Electrocardiogram (ECG/EKG): To check the heart's electrical activity.
Electrocardiogram (ECG/EKG): To check the heart's electrical activity.![]()

![]() Echocardiogram: An ultrasound of the heart to assess its structure and function.
Echocardiogram: An ultrasound of the heart to assess its structure and function.![]()

![]() Blood Tests: Including markers of heart damage (troponin), inflammation (ESR, CRP), and tests to look for infections or autoimmune conditions.
Blood Tests: Including markers of heart damage (troponin), inflammation (ESR, CRP), and tests to look for infections or autoimmune conditions.![]()

![]() Cardiac MRI: A detailed imaging test that can detect inflammation in the heart muscle.
Cardiac MRI: A detailed imaging test that can detect inflammation in the heart muscle.![]()

![]() Endomyocardial Biopsy: In some cases, a small sample of heart muscle is taken and examined under a microscope. This is the most definitive test but is not always necessary.
Endomyocardial Biopsy: In some cases, a small sample of heart muscle is taken and examined under a microscope. This is the most definitive test but is not always necessary.
![]() Treatment: Treatment focuses on reducing inflammation and supporting the heart's function.
Treatment: Treatment focuses on reducing inflammation and supporting the heart's function.![]()

![]() Medications:
Medications:![]()

![]() Anti-inflammatory drugs: Such as corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs). (Note: NSAIDs can sometimes worsen myocarditis, so they should be used with caution and under medical supervision).
Anti-inflammatory drugs: Such as corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs). (Note: NSAIDs can sometimes worsen myocarditis, so they should be used with caution and under medical supervision).![]()

![]() Medications for heart failure: Such as ACE inhibitors, beta-blockers, and diuretics.
Medications for heart failure: Such as ACE inhibitors, beta-blockers, and diuretics.![]()

![]() Antiarrhythmic drugs: To control irregular heartbeats.
Antiarrhythmic drugs: To control irregular heartbeats.![]()

![]() Immunosuppressants: May be used in autoimmune-related myocarditis.
Immunosuppressants: May be used in autoimmune-related myocarditis.![]()

![]() Antibiotics, antivirals, or antifungals: If the myocarditis is caused by an infection.
Antibiotics, antivirals, or antifungals: If the myocarditis is caused by an infection.![]()

![]() Lifestyle Changes:
Lifestyle Changes:![]()

![]() Rest: Important to allow the heart to recover.
Rest: Important to allow the heart to recover.![]()

![]() Low-sodium diet: To help reduce fluid retention.
Low-sodium diet: To help reduce fluid retention.![]()

![]() Avoiding strenuous activity: Until cleared by a doctor.
Avoiding strenuous activity: Until cleared by a doctor.![]()

![]() In severe cases:
In severe cases:![]()

![]() Hospitalization: For close monitoring and treatment.
Hospitalization: For close monitoring and treatment.![]()

![]() Mechanical support: Such as a ventricular assist device (VAD) to help the heart pump blood.
Mechanical support: Such as a ventricular assist device (VAD) to help the heart pump blood.![]()

![]() Heart transplant: In rare cases of severe, irreversible heart damage.
Heart transplant: In rare cases of severe, irreversible heart damage.
![]() Prognosis: The outcome of myocarditis varies. Many people recover completely, while others may develop chronic heart problems, such as heart failure or arrhythmias. The prognosis depends on the severity of the inflammation, the underlying cause, and how quickly treatment is started.
Prognosis: The outcome of myocarditis varies. Many people recover completely, while others may develop chronic heart problems, such as heart failure or arrhythmias. The prognosis depends on the severity of the inflammation, the underlying cause, and how quickly treatment is started.
Important Considerations:
![]() COVID-19 and mRNA vaccines: While myocarditis has been linked to both COVID-19 and mRNA vaccines, it's generally considered rare. The risk of myocarditis from a COVID-19 infection is significantly higher than from vaccination. The benefits of vaccination in preventing severe COVID-19 outweigh the risk of myocarditis.
COVID-19 and mRNA vaccines: While myocarditis has been linked to both COVID-19 and mRNA vaccines, it's generally considered rare. The risk of myocarditis from a COVID-19 infection is significantly higher than from vaccination. The benefits of vaccination in preventing severe COVID-19 outweigh the risk of myocarditis.
![]() Seek medical attention: If you experience symptoms of myocarditis, it's important to see a doctor promptly for diagnosis and treatment.
Seek medical attention: If you experience symptoms of myocarditis, it's important to see a doctor promptly for diagnosis and treatment.
This information is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.