Myotonic dystrophy
Published: 18 Jun 2025
ICD9: 359.21 ICD10: G71.11 ICD11: 8C71.0
Myotonic dystrophy (DM) is a form of muscular dystrophy characterized by myotonia (prolonged muscle contraction) and progressive muscle weakness and wasting.
It's a multisystem disorder, meaning it affects various parts of the body in addition to muscles.
Here's a breakdown of key aspects of myotonic dystrophy:
Key Features:
![]() Myotonia: This is the hallmark of DM. It's the delayed relaxation of muscles after contraction. People with DM may have difficulty releasing their grip, relaxing their facial muscles, or releasing their tongue after sticking it out. It is often worse after inactivity and in cold weather.
Myotonia: This is the hallmark of DM. It's the delayed relaxation of muscles after contraction. People with DM may have difficulty releasing their grip, relaxing their facial muscles, or releasing their tongue after sticking it out. It is often worse after inactivity and in cold weather.
![]() Progressive Muscle Weakness and Wasting: This worsens over time and primarily affects:
Progressive Muscle Weakness and Wasting: This worsens over time and primarily affects:![]()

![]() Distal muscles: Hands, feet, lower legs, and forearms are often affected first.
Distal muscles: Hands, feet, lower legs, and forearms are often affected first.![]()

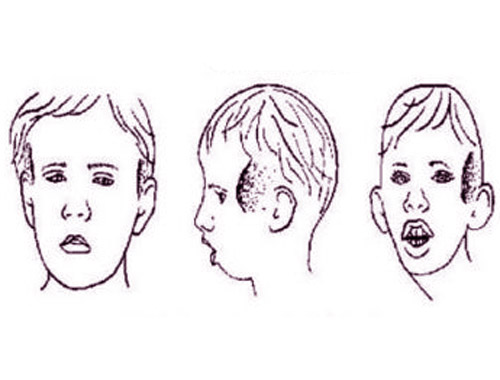
![]() Facial muscles: Leading to a characteristic "long face" or "hatchet face."
Facial muscles: Leading to a characteristic "long face" or "hatchet face."![]()

![]() Neck muscles: Causing difficulty holding the head up.
Neck muscles: Causing difficulty holding the head up.![]()

![]() Other muscles: Depending on the type and severity of the condition.
Other muscles: Depending on the type and severity of the condition.
![]() Multisystem Involvement: DM can affect various organs and systems, including:
Multisystem Involvement: DM can affect various organs and systems, including:![]()

![]() Heart: Cardiac arrhythmias, cardiomyopathy.
Heart: Cardiac arrhythmias, cardiomyopathy.![]()

![]() Eyes: Cataracts, which often develop early in life.
Eyes: Cataracts, which often develop early in life.![]()

![]() Endocrine system: Diabetes, thyroid problems.
Endocrine system: Diabetes, thyroid problems.![]()

![]() Gastrointestinal system: Difficulty swallowing (dysphagia), constipation, and irritable bowel syndrome (IBS).
Gastrointestinal system: Difficulty swallowing (dysphagia), constipation, and irritable bowel syndrome (IBS).![]()

![]() Brain: Cognitive impairment, excessive daytime sleepiness, behavioral changes.
Brain: Cognitive impairment, excessive daytime sleepiness, behavioral changes.![]()

![]() Respiratory system: Weakness of respiratory muscles, leading to breathing problems, especially at night.
Respiratory system: Weakness of respiratory muscles, leading to breathing problems, especially at night.![]()

![]() Reproductive system: In males, testicular atrophy and infertility; in females, menstrual irregularities and difficulty with pregnancy.
Reproductive system: In males, testicular atrophy and infertility; in females, menstrual irregularities and difficulty with pregnancy.
Types:
There are two main types of myotonic dystrophy:
![]() Myotonic Dystrophy Type 1 (DM1): This is the more common and usually more severe form. It's caused by an expansion of a CTG repeat in the *DMPK* gene. The size of the repeat correlates with the severity and age of onset of the disease. Larger repeats tend to cause earlier onset and more severe symptoms.
Myotonic Dystrophy Type 1 (DM1): This is the more common and usually more severe form. It's caused by an expansion of a CTG repeat in the *DMPK* gene. The size of the repeat correlates with the severity and age of onset of the disease. Larger repeats tend to cause earlier onset and more severe symptoms.
![]() Myotonic Dystrophy Type 2 (DM2): Also known as proximal myotonic myopathy (PROMM). It's caused by an expansion of a CCTG repeat in the *CNBP* gene. DM2 tends to be milder than DM1, with less prominent myotonia and a later onset. Muscle weakness is typically more proximal (closer to the trunk) than distal.
Myotonic Dystrophy Type 2 (DM2): Also known as proximal myotonic myopathy (PROMM). It's caused by an expansion of a CCTG repeat in the *CNBP* gene. DM2 tends to be milder than DM1, with less prominent myotonia and a later onset. Muscle weakness is typically more proximal (closer to the trunk) than distal.
Genetics:
![]() Both DM1 and DM2 are inherited in an autosomal dominant pattern. This means that only one copy of the mutated gene is needed to cause the disorder. If one parent has DM, there's a 50% chance their child will inherit the condition.
Both DM1 and DM2 are inherited in an autosomal dominant pattern. This means that only one copy of the mutated gene is needed to cause the disorder. If one parent has DM, there's a 50% chance their child will inherit the condition.
![]() Anticipation: A key feature of DM1 is *anticipation*. This means that the severity of the disease tends to increase and the age of onset tends to decrease in successive generations. This is because the CTG repeat expansion can become larger when passed from parent to child, especially from mother to child. Anticipation is less pronounced in DM2.
Anticipation: A key feature of DM1 is *anticipation*. This means that the severity of the disease tends to increase and the age of onset tends to decrease in successive generations. This is because the CTG repeat expansion can become larger when passed from parent to child, especially from mother to child. Anticipation is less pronounced in DM2.
Diagnosis:
![]() Clinical Examination: Based on symptoms like myotonia, muscle weakness, and other associated features.
Clinical Examination: Based on symptoms like myotonia, muscle weakness, and other associated features.
![]() Electromyography (EMG): A test that measures the electrical activity of muscles. It can detect the characteristic myotonic discharges.
Electromyography (EMG): A test that measures the electrical activity of muscles. It can detect the characteristic myotonic discharges.
![]() Genetic Testing: A blood test to confirm the diagnosis by identifying the expanded CTG or CCTG repeat in the *DMPK* or *CNBP* gene, respectively.
Genetic Testing: A blood test to confirm the diagnosis by identifying the expanded CTG or CCTG repeat in the *DMPK* or *CNBP* gene, respectively.
![]() Muscle Biopsy: May be used, but genetic testing is the preferred method of diagnosis.
Muscle Biopsy: May be used, but genetic testing is the preferred method of diagnosis.
Treatment:
There is no cure for myotonic dystrophy. Treatment focuses on managing symptoms and improving quality of life.
![]() Myotonia: Medications like mexiletine, phenytoin, or quinine can help reduce muscle stiffness.
Myotonia: Medications like mexiletine, phenytoin, or quinine can help reduce muscle stiffness.
![]() Muscle Weakness: Physical therapy and occupational therapy can help maintain muscle strength and function. Assistive devices may be needed as the disease progresses.
Muscle Weakness: Physical therapy and occupational therapy can help maintain muscle strength and function. Assistive devices may be needed as the disease progresses.
![]() Cardiac Problems: Regular monitoring and treatment of arrhythmias or heart failure.
Cardiac Problems: Regular monitoring and treatment of arrhythmias or heart failure.
![]() Cataracts: Surgical removal.
Cataracts: Surgical removal.
![]() Endocrine Problems: Management of diabetes or thyroid problems.
Endocrine Problems: Management of diabetes or thyroid problems.
![]() Sleep Disorders: Treatment for excessive daytime sleepiness or sleep apnea.
Sleep Disorders: Treatment for excessive daytime sleepiness or sleep apnea.
![]() Other Symptoms: Treatment is tailored to address specific symptoms as they arise.
Other Symptoms: Treatment is tailored to address specific symptoms as they arise.
![]() Regular monitoring: Regular checkups with a neurologist, cardiologist, ophthalmologist, and other specialists are important for managing the various aspects of the disease.
Regular monitoring: Regular checkups with a neurologist, cardiologist, ophthalmologist, and other specialists are important for managing the various aspects of the disease.
Prognosis:
The prognosis for people with myotonic dystrophy varies depending on the type and severity of the condition. Some individuals may have mild symptoms and live a normal lifespan, while others may experience more significant disability and a shorter lifespan due to complications such as cardiac or respiratory failure.
Important Considerations:
![]() Genetic Counseling: Genetic counseling is important for families with a history of myotonic dystrophy to understand the risks of inheritance and discuss reproductive options.
Genetic Counseling: Genetic counseling is important for families with a history of myotonic dystrophy to understand the risks of inheritance and discuss reproductive options.
![]() Early Diagnosis: Early diagnosis and management can help improve quality of life and prevent complications.
Early Diagnosis: Early diagnosis and management can help improve quality of life and prevent complications.
![]() Multidisciplinary Care: People with myotonic dystrophy benefit from a multidisciplinary team of healthcare professionals.
Multidisciplinary Care: People with myotonic dystrophy benefit from a multidisciplinary team of healthcare professionals.
In summary, myotonic dystrophy is a complex genetic disorder with variable presentation and multisystem involvement. Understanding its different aspects is crucial for accurate diagnosis, appropriate management, and improved patient outcomes.