Neuroblastoma cancer
Published: 18 Jun 2025
ICD9: 194.0 ICD10: C74.90 ICD11: XH85Z0
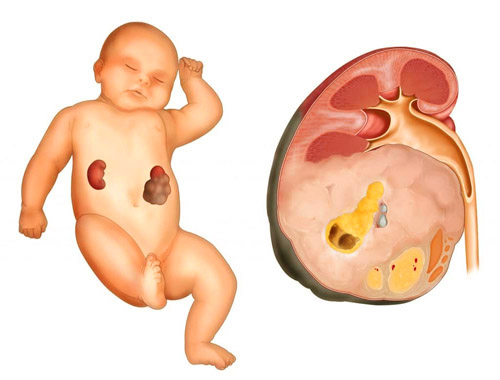
Neuroblastoma is a type of cancer that develops from immature nerve cells called neuroblasts.
These cells are supposed to mature into nerve cells. Instead, they can grow out of control and form a tumor. It's most common in children, typically under the age of 5, but can rarely occur in older children and adults.
Here's a more detailed breakdown:
![]() Origin: Neuroblastoma arises from the sympathetic nervous system, which controls many automatic functions in the body, like heart rate, blood pressure, digestion, and stress responses. These neuroblasts are found in several areas of the body during fetal development, but normally mature or disappear shortly after birth.
Origin: Neuroblastoma arises from the sympathetic nervous system, which controls many automatic functions in the body, like heart rate, blood pressure, digestion, and stress responses. These neuroblasts are found in several areas of the body during fetal development, but normally mature or disappear shortly after birth.
![]() Common Locations:
Common Locations:![]()

![]() Adrenal glands: These glands sit atop the kidneys and are the most frequent site of neuroblastoma.
Adrenal glands: These glands sit atop the kidneys and are the most frequent site of neuroblastoma.![]()

![]() Abdomen: Along the sympathetic nerve chains.
Abdomen: Along the sympathetic nerve chains.![]()

![]() Chest: In the nerve tissues along the spine.
Chest: In the nerve tissues along the spine.![]()

![]() Neck: Less commonly.
Neck: Less commonly.![]()

![]() Spinal Cord: Rarely.
Spinal Cord: Rarely.
![]() Spread (Metastasis): Neuroblastoma can spread to other parts of the body, including:
Spread (Metastasis): Neuroblastoma can spread to other parts of the body, including:![]()

![]() Lymph nodes
Lymph nodes![]()

![]() Bones
Bones![]()

![]() Bone marrow
Bone marrow![]()

![]() Liver
Liver![]()

![]() Skin (particularly in infants)
Skin (particularly in infants)
![]() Symptoms: The symptoms of neuroblastoma vary widely depending on the location of the tumor and whether it has spread. Some common symptoms include:
Symptoms: The symptoms of neuroblastoma vary widely depending on the location of the tumor and whether it has spread. Some common symptoms include:![]()

![]() General symptoms:
General symptoms:![]()

![]() Fatigue
Fatigue![]()

![]() Loss of appetite
Loss of appetite![]()

![]() Fever
Fever![]()

![]() Tumor-related symptoms:
Tumor-related symptoms:![]()

![]() A lump or swelling in the abdomen, neck, or chest
A lump or swelling in the abdomen, neck, or chest![]()

![]() Bone pain
Bone pain![]()

![]() Unexplained weight loss
Unexplained weight loss![]()

![]() Constipation or changes in bowel habits
Constipation or changes in bowel habits![]()

![]() Difficulty breathing (if the tumor is pressing on the airway)
Difficulty breathing (if the tumor is pressing on the airway)![]()

![]() Drooping eyelid, small pupil, and decreased sweating on one side of the face (Horner's syndrome, if the tumor affects nerves in the neck)
Drooping eyelid, small pupil, and decreased sweating on one side of the face (Horner's syndrome, if the tumor affects nerves in the neck)![]()

![]() Weakness or paralysis in the legs (if the tumor presses on the spinal cord)
Weakness or paralysis in the legs (if the tumor presses on the spinal cord)![]()

![]() Swollen belly
Swollen belly![]()

![]() Symptoms from hormones produced by the tumor (less common):
Symptoms from hormones produced by the tumor (less common):![]()

![]() Diarrhea
Diarrhea![]()

![]() High blood pressure
High blood pressure![]()

![]() Rapid heart rate
Rapid heart rate![]()

![]() Skin flushing
Skin flushing
![]() Causes: The exact cause of neuroblastoma is not fully understood. Most cases are not inherited. A very small percentage are linked to genetic mutations passed down from parents.
Causes: The exact cause of neuroblastoma is not fully understood. Most cases are not inherited. A very small percentage are linked to genetic mutations passed down from parents.
![]() Diagnosis: Diagnosis typically involves:
Diagnosis: Diagnosis typically involves:![]()

![]() Physical exam: To check for lumps or other abnormalities.
Physical exam: To check for lumps or other abnormalities.![]()

![]() Imaging tests: X-rays, CT scans, MRI scans, and MIBG scans (metaiodobenzylguanidine, a radioactive substance absorbed by neuroblastoma cells) help locate and assess the tumor.
Imaging tests: X-rays, CT scans, MRI scans, and MIBG scans (metaiodobenzylguanidine, a radioactive substance absorbed by neuroblastoma cells) help locate and assess the tumor.![]()

![]() Biopsy: A sample of the tumor is taken and examined under a microscope to confirm the diagnosis.
Biopsy: A sample of the tumor is taken and examined under a microscope to confirm the diagnosis.![]()

![]() Bone marrow aspiration and biopsy: To check for the spread of cancer to the bone marrow.
Bone marrow aspiration and biopsy: To check for the spread of cancer to the bone marrow.![]()

![]() Urine tests: To measure levels of certain substances (catecholamines) produced by neuroblastoma cells.
Urine tests: To measure levels of certain substances (catecholamines) produced by neuroblastoma cells.![]()

![]() Genetic testing: To look for specific genetic mutations that may affect the prognosis and treatment.
Genetic testing: To look for specific genetic mutations that may affect the prognosis and treatment.
![]() Staging: Neuroblastoma is staged to determine the extent of the cancer and help guide treatment decisions. Several staging systems exist, with the International Neuroblastoma Staging System (INSS) being one of the most common. Factors considered in staging include tumor size, location, whether the tumor has spread to nearby lymph nodes or distant sites, and certain genetic markers.
Staging: Neuroblastoma is staged to determine the extent of the cancer and help guide treatment decisions. Several staging systems exist, with the International Neuroblastoma Staging System (INSS) being one of the most common. Factors considered in staging include tumor size, location, whether the tumor has spread to nearby lymph nodes or distant sites, and certain genetic markers.
![]() Treatment: Treatment for neuroblastoma depends on several factors, including the child's age, the stage of the cancer, genetic features of the tumor, and the child's overall health. Treatment options may include:
Treatment: Treatment for neuroblastoma depends on several factors, including the child's age, the stage of the cancer, genetic features of the tumor, and the child's overall health. Treatment options may include:![]()

![]() Surgery: To remove the tumor.
Surgery: To remove the tumor.![]()

![]() Chemotherapy: To kill cancer cells.
Chemotherapy: To kill cancer cells.![]()

![]() Radiation therapy: To kill cancer cells using high-energy rays.
Radiation therapy: To kill cancer cells using high-energy rays.![]()

![]() Stem cell transplant: To replace damaged bone marrow with healthy cells.
Stem cell transplant: To replace damaged bone marrow with healthy cells.![]()

![]() Immunotherapy: To boost the body's immune system to fight cancer cells.
Immunotherapy: To boost the body's immune system to fight cancer cells.![]()

![]() Targeted therapy: Drugs that target specific vulnerabilities in cancer cells.
Targeted therapy: Drugs that target specific vulnerabilities in cancer cells.![]()

![]() Observation: In some low-risk cases, the tumor may be monitored closely without immediate treatment.
Observation: In some low-risk cases, the tumor may be monitored closely without immediate treatment.
![]() Prognosis: The prognosis for neuroblastoma varies widely depending on the stage of the cancer, the child's age, and certain genetic factors. High-risk neuroblastoma can be very difficult to treat. Factors that may affect prognosis include:
Prognosis: The prognosis for neuroblastoma varies widely depending on the stage of the cancer, the child's age, and certain genetic factors. High-risk neuroblastoma can be very difficult to treat. Factors that may affect prognosis include:![]()

![]() Age: Younger children generally have a better prognosis than older children.
Age: Younger children generally have a better prognosis than older children.![]()

![]() Stage: Early-stage neuroblastoma has a better prognosis than advanced-stage neuroblastoma.
Stage: Early-stage neuroblastoma has a better prognosis than advanced-stage neuroblastoma.![]()

![]() MYCN amplification: Amplification of the MYCN gene is associated with a poorer prognosis.
MYCN amplification: Amplification of the MYCN gene is associated with a poorer prognosis.![]()

![]() DNA ploidy: Tumors with hyperdiploidy (more than the normal number of chromosomes) tend to have a better prognosis.
DNA ploidy: Tumors with hyperdiploidy (more than the normal number of chromosomes) tend to have a better prognosis.![]()

![]() Histology: The appearance of the tumor cells under a microscope can provide information about the prognosis.
Histology: The appearance of the tumor cells under a microscope can provide information about the prognosis.
![]() Research: There is ongoing research into new and more effective treatments for neuroblastoma, including targeted therapies, immunotherapies, and improved ways to predict and manage the disease.
Research: There is ongoing research into new and more effective treatments for neuroblastoma, including targeted therapies, immunotherapies, and improved ways to predict and manage the disease.
Important Note: This information is for general knowledge and educational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment. If you suspect your child has neuroblastoma, seek immediate medical attention. Early diagnosis and treatment are crucial for improving outcomes.