Osteoarthritis
Published: 18 Jun 2025
ICD9: 715.96 ICD10: M17.9 ICD11: FA2Z
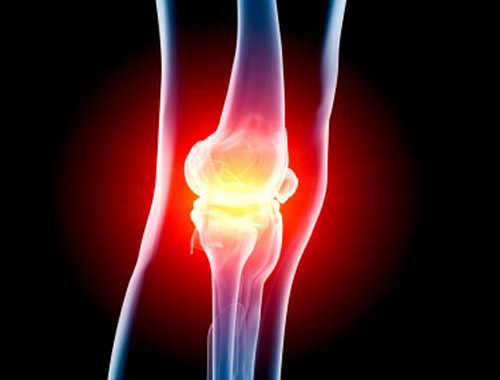
Osteoarthritis (OA) is the most common form of arthritis, affecting millions of people worldwide.
It's a degenerative joint disease characterized by the breakdown of cartilage in the joints. Here's a more detailed breakdown:
What is Cartilage?
![]() Cartilage is a firm, slippery tissue that covers the ends of bones in a joint.
Cartilage is a firm, slippery tissue that covers the ends of bones in a joint.
![]() It acts as a cushion, allowing the bones to glide smoothly over each other during movement.
It acts as a cushion, allowing the bones to glide smoothly over each other during movement.
![]() It also helps absorb shock when pressure is applied to the joint.
It also helps absorb shock when pressure is applied to the joint.
What Happens in Osteoarthritis?
1. Cartilage Breakdown: In OA, the cartilage gradually breaks down and wears away.
2. Bone on Bone: As the cartilage thins, there is less protection for the bones. Eventually, bone may rub directly on bone.
3. Joint Changes:![]()

![]() The joint space narrows.
The joint space narrows.![]()

![]() The bones may thicken and develop bony growths called bone spurs (osteophytes) around the joint.
The bones may thicken and develop bony growths called bone spurs (osteophytes) around the joint.![]()

![]() The lining of the joint (synovium) may become inflamed and produce excess fluid.
The lining of the joint (synovium) may become inflamed and produce excess fluid.
4. Pain and Reduced Mobility: These changes lead to pain, stiffness, swelling, and reduced range of motion in the affected joint.
Key Characteristics of Osteoarthritis:
![]() Degenerative: It gets worse over time.
Degenerative: It gets worse over time.
![]() Non-inflammatory (initially): While inflammation can occur as a secondary symptom, OA is primarily a degenerative condition, unlike rheumatoid arthritis which is primarily inflammatory.
Non-inflammatory (initially): While inflammation can occur as a secondary symptom, OA is primarily a degenerative condition, unlike rheumatoid arthritis which is primarily inflammatory.
![]() Localized: Typically affects individual joints, rather than being systemic (affecting the whole body).
Localized: Typically affects individual joints, rather than being systemic (affecting the whole body).
Commonly Affected Joints:
![]() Knees
Knees
![]() Hips
Hips
![]() Hands (fingers and thumbs)
Hands (fingers and thumbs)
![]() Spine (especially the neck and lower back)
Spine (especially the neck and lower back)
Symptoms of Osteoarthritis:
![]() Pain: Joint pain that worsens with activity and improves with rest (initially). As OA progresses, pain may be present even at rest.
Pain: Joint pain that worsens with activity and improves with rest (initially). As OA progresses, pain may be present even at rest.
![]() Stiffness: Joint stiffness, especially in the morning or after a period of inactivity.
Stiffness: Joint stiffness, especially in the morning or after a period of inactivity.
![]() Swelling: Inflammation and fluid buildup in the joint.
Swelling: Inflammation and fluid buildup in the joint.
![]() Tenderness: Pain when touching the joint.
Tenderness: Pain when touching the joint.
![]() Loss of flexibility: Decreased range of motion in the joint.
Loss of flexibility: Decreased range of motion in the joint.
![]() Grating sensation: A feeling or sound of bones rubbing together (crepitus) during movement.
Grating sensation: A feeling or sound of bones rubbing together (crepitus) during movement.
![]() Bone spurs: Hard lumps may form around the joint.
Bone spurs: Hard lumps may form around the joint.
Causes and Risk Factors:
While the exact cause isn't always clear, several factors increase the risk of developing OA:
![]() Age: The risk increases with age as cartilage naturally wears down over time.
Age: The risk increases with age as cartilage naturally wears down over time.
![]() Genetics: A family history of OA can increase your risk.
Genetics: A family history of OA can increase your risk.
![]() Obesity: Excess weight puts more stress on weight-bearing joints like the knees and hips.
Obesity: Excess weight puts more stress on weight-bearing joints like the knees and hips.
![]() Joint injuries: Previous injuries to a joint, such as fractures or ligament tears, can increase the risk of OA later in life.
Joint injuries: Previous injuries to a joint, such as fractures or ligament tears, can increase the risk of OA later in life.
![]() Repetitive stress: Jobs or activities that involve repetitive motions can put stress on certain joints.
Repetitive stress: Jobs or activities that involve repetitive motions can put stress on certain joints.
![]() Bone deformities: Conditions like bowlegs or knock-knees can increase the risk of OA.
Bone deformities: Conditions like bowlegs or knock-knees can increase the risk of OA.
![]() Certain medical conditions: Diabetes, hemochromatosis, and other conditions can increase the risk.
Certain medical conditions: Diabetes, hemochromatosis, and other conditions can increase the risk.
Diagnosis:
![]() Physical Exam: Doctor will examine the affected joint for tenderness, swelling, range of motion, and stability.
Physical Exam: Doctor will examine the affected joint for tenderness, swelling, range of motion, and stability.
![]() X-rays: Can show cartilage loss, bone spurs, and joint space narrowing.
X-rays: Can show cartilage loss, bone spurs, and joint space narrowing.
![]() MRI (Magnetic Resonance Imaging): Provides more detailed images of the joint, including cartilage, ligaments, and tendons.
MRI (Magnetic Resonance Imaging): Provides more detailed images of the joint, including cartilage, ligaments, and tendons.
![]() Joint Fluid Analysis: A sample of fluid may be taken from the joint to rule out other conditions, such as infection or gout.
Joint Fluid Analysis: A sample of fluid may be taken from the joint to rule out other conditions, such as infection or gout.
Treatment:
There is no cure for OA, but various treatments can help manage pain and improve function:
![]() Lifestyle modifications:
Lifestyle modifications:![]()

![]() Weight loss (if overweight or obese)
Weight loss (if overweight or obese)![]()

![]() Exercise (low-impact activities like swimming, walking, and cycling)
Exercise (low-impact activities like swimming, walking, and cycling)![]()

![]() Rest and activity balance
Rest and activity balance![]()

![]() Assistive devices (canes, walkers, braces)
Assistive devices (canes, walkers, braces)
![]() Medications:
Medications:![]()

![]() Over-the-counter pain relievers (acetaminophen, NSAIDs)
Over-the-counter pain relievers (acetaminophen, NSAIDs)![]()

![]() Prescription NSAIDs (stronger than over-the-counter)
Prescription NSAIDs (stronger than over-the-counter)![]()

![]() Corticosteroid injections (to reduce inflammation)
Corticosteroid injections (to reduce inflammation)![]()

![]() Hyaluronic acid injections (to lubricate the joint)
Hyaluronic acid injections (to lubricate the joint)![]()

![]() Duloxetine (a medication also used for depression, that can help with chronic pain)
Duloxetine (a medication also used for depression, that can help with chronic pain)
![]() Physical therapy: To strengthen muscles around the joint, improve range of motion, and reduce pain.
Physical therapy: To strengthen muscles around the joint, improve range of motion, and reduce pain.
![]() Occupational therapy: To learn ways to perform daily activities with less stress on the joints.
Occupational therapy: To learn ways to perform daily activities with less stress on the joints.
![]() Surgery:
Surgery:![]()

![]() Joint replacement (arthroplasty): Replacing the damaged joint with an artificial joint. Most commonly performed on hips and knees.
Joint replacement (arthroplasty): Replacing the damaged joint with an artificial joint. Most commonly performed on hips and knees.![]()

![]() Arthroscopy: A minimally invasive procedure to clean out loose cartilage or bone spurs.
Arthroscopy: A minimally invasive procedure to clean out loose cartilage or bone spurs.![]()

![]() Osteotomy: Realigning the bone to reduce stress on the joint.
Osteotomy: Realigning the bone to reduce stress on the joint.
In summary, Osteoarthritis is a common condition that causes joint pain and stiffness due to the breakdown of cartilage. While it can't be cured, various treatments can help manage the symptoms and improve quality of life.
It's crucial to consult a doctor if you suspect you have osteoarthritis. They can provide an accurate diagnosis and recommend the most appropriate treatment plan for your individual needs.