Osteoporosis
Published: 18 Jun 2025
ICD9: 733.00 ICD10: M81.0 ICD11: FB83.1
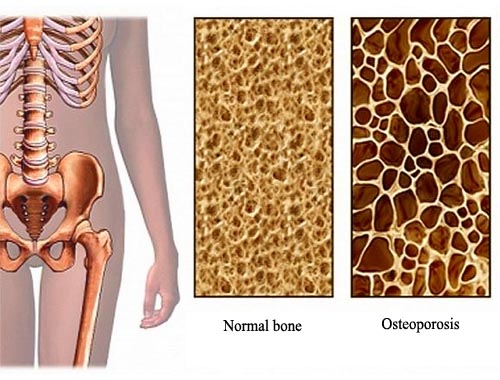
Osteoporosis is a disease that weakens bones, making them more likely to break.
It literally means "porous bone." Here's a breakdown of what you need to know:
Key Characteristics:
![]() Reduced Bone Density: Bone is living tissue that is constantly being broken down and replaced. In osteoporosis, the body either loses bone faster than it makes new bone, or both. This leads to a decrease in bone density.
Reduced Bone Density: Bone is living tissue that is constantly being broken down and replaced. In osteoporosis, the body either loses bone faster than it makes new bone, or both. This leads to a decrease in bone density.
![]() Increased Risk of Fractures: As bones become more porous and fragile, they are more susceptible to fractures, especially in the hip, spine, wrist, and shoulder. These fractures can occur from minor falls or even everyday activities.
Increased Risk of Fractures: As bones become more porous and fragile, they are more susceptible to fractures, especially in the hip, spine, wrist, and shoulder. These fractures can occur from minor falls or even everyday activities.
![]() Often No Symptoms Until a Fracture: Osteoporosis is often called a "silent disease" because most people don't know they have it until they break a bone.
Often No Symptoms Until a Fracture: Osteoporosis is often called a "silent disease" because most people don't know they have it until they break a bone.
![]() Microarchitectural Deterioration: It's not just about the amount of bone, but also the structure. In osteoporosis, the internal architecture of the bone deteriorates, making it weaker.
Microarchitectural Deterioration: It's not just about the amount of bone, but also the structure. In osteoporosis, the internal architecture of the bone deteriorates, making it weaker.
Causes and Risk Factors:
![]() Age: Bone density naturally decreases with age.
Age: Bone density naturally decreases with age.
![]() Gender: Women are more likely to develop osteoporosis than men, especially after menopause due to the decrease in estrogen.
Gender: Women are more likely to develop osteoporosis than men, especially after menopause due to the decrease in estrogen.
![]() Race: White and Asian women are at higher risk.
Race: White and Asian women are at higher risk.
![]() Family History: Having a parent or sibling with osteoporosis increases your risk.
Family History: Having a parent or sibling with osteoporosis increases your risk.
![]() Body Size: Small-framed individuals tend to have less bone mass and are at higher risk.
Body Size: Small-framed individuals tend to have less bone mass and are at higher risk.
![]() Hormone Levels:
Hormone Levels:![]()

![]() Estrogen: Low estrogen levels (often due to menopause) are a major risk factor.
Estrogen: Low estrogen levels (often due to menopause) are a major risk factor.![]()

![]() Testosterone: Low testosterone levels in men can also contribute to osteoporosis.
Testosterone: Low testosterone levels in men can also contribute to osteoporosis.![]()

![]() Thyroid Hormones: An overactive thyroid can cause bone loss.
Thyroid Hormones: An overactive thyroid can cause bone loss.
![]() Diet: Low calcium and vitamin D intake can increase the risk.
Diet: Low calcium and vitamin D intake can increase the risk.
![]() Medical Conditions: Certain medical conditions, such as celiac disease, inflammatory bowel disease, kidney disease, and rheumatoid arthritis, can increase the risk.
Medical Conditions: Certain medical conditions, such as celiac disease, inflammatory bowel disease, kidney disease, and rheumatoid arthritis, can increase the risk.
![]() Medications: Long-term use of certain medications, such as corticosteroids (e.g., prednisone), some anti-seizure medications, and some cancer treatments, can increase the risk.
Medications: Long-term use of certain medications, such as corticosteroids (e.g., prednisone), some anti-seizure medications, and some cancer treatments, can increase the risk.
![]() Lifestyle Factors:
Lifestyle Factors:![]()

![]() Sedentary Lifestyle: Lack of weight-bearing exercise weakens bones.
Sedentary Lifestyle: Lack of weight-bearing exercise weakens bones.![]()

![]() Excessive Alcohol Consumption: Can interfere with calcium absorption.
Excessive Alcohol Consumption: Can interfere with calcium absorption.![]()

![]() Tobacco Use: Weakens bones.
Tobacco Use: Weakens bones.
Diagnosis:
![]() Bone Density Test (DEXA Scan): This is the most common test used to diagnose osteoporosis. It measures bone density in the hip and spine. The results are reported as a T-score.
Bone Density Test (DEXA Scan): This is the most common test used to diagnose osteoporosis. It measures bone density in the hip and spine. The results are reported as a T-score.![]()

![]() T-score -1.0 or higher: Normal bone density
T-score -1.0 or higher: Normal bone density![]()

![]() T-score between -1.0 and -2.5: Osteopenia (low bone density, but not yet osteoporosis)
T-score between -1.0 and -2.5: Osteopenia (low bone density, but not yet osteoporosis)![]()

![]() T-score -2.5 or lower: Osteoporosis
T-score -2.5 or lower: Osteoporosis
Treatment and Prevention:
![]() Medications: Several medications are available to treat osteoporosis, including:
Medications: Several medications are available to treat osteoporosis, including:![]()

![]() Bisphosphonates: Slow bone loss.
Bisphosphonates: Slow bone loss.![]()

![]() RANK Ligand Inhibitor (Denosumab): Reduces bone resorption.
RANK Ligand Inhibitor (Denosumab): Reduces bone resorption.![]()

![]() Selective Estrogen Receptor Modulators (SERMs): Mimic the effects of estrogen on bone.
Selective Estrogen Receptor Modulators (SERMs): Mimic the effects of estrogen on bone.![]()

![]() Anabolic Medications: Stimulate bone formation.
Anabolic Medications: Stimulate bone formation.
![]() Lifestyle Changes:
Lifestyle Changes:![]()

![]() Calcium and Vitamin D: Ensure adequate intake through diet and supplements.
Calcium and Vitamin D: Ensure adequate intake through diet and supplements.![]()

![]() Weight-Bearing Exercise: Activities like walking, jogging, dancing, and weightlifting help build and maintain bone density.
Weight-Bearing Exercise: Activities like walking, jogging, dancing, and weightlifting help build and maintain bone density.![]()

![]() Fall Prevention: Take steps to prevent falls, such as removing hazards in the home, using assistive devices, and improving balance.
Fall Prevention: Take steps to prevent falls, such as removing hazards in the home, using assistive devices, and improving balance.![]()

![]() Quit Smoking: Smoking is detrimental to bone health.
Quit Smoking: Smoking is detrimental to bone health.![]()

![]() Limit Alcohol Consumption: Excessive alcohol intake can harm bones.
Limit Alcohol Consumption: Excessive alcohol intake can harm bones.
In summary, osteoporosis is a common and serious condition that weakens bones and increases the risk of fractures. Early detection and treatment are crucial to preventing fractures and maintaining quality of life. Consult with your doctor to assess your risk factors and discuss appropriate screening and prevention strategies.