Pancreatitis
Published: 18 Jun 2025
ICD9: 577.0 ICD10: K85.9 ICD11: DC31
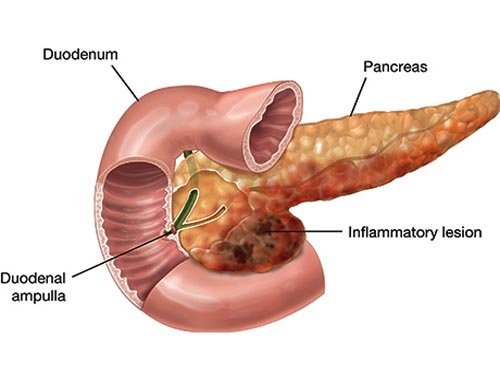
Pancreatitis is an inflammation of the pancreas.
The pancreas is a gland located behind the stomach that produces enzymes that help digest food and hormones that regulate blood sugar.
Here's a breakdown:
What the Pancreas Does:
![]() Digestive Enzymes: The pancreas secretes enzymes that break down proteins, carbohydrates, and fats in the small intestine. These enzymes travel through a duct (the pancreatic duct) to reach the small intestine.
Digestive Enzymes: The pancreas secretes enzymes that break down proteins, carbohydrates, and fats in the small intestine. These enzymes travel through a duct (the pancreatic duct) to reach the small intestine.
![]() Hormones: The pancreas produces hormones, like insulin and glucagon, that regulate blood sugar levels. These hormones are secreted directly into the bloodstream.
Hormones: The pancreas produces hormones, like insulin and glucagon, that regulate blood sugar levels. These hormones are secreted directly into the bloodstream.
What Happens in Pancreatitis:
In pancreatitis, digestive enzymes become activated *inside* the pancreas instead of traveling to the small intestine. This leads to the pancreas essentially digesting itself, causing inflammation, pain, and potential damage.
Types of Pancreatitis:
![]() Acute Pancreatitis: This is a sudden inflammation of the pancreas. Symptoms are usually severe and appear quickly. It's often caused by gallstones or heavy alcohol use. Most people with acute pancreatitis recover fully.
Acute Pancreatitis: This is a sudden inflammation of the pancreas. Symptoms are usually severe and appear quickly. It's often caused by gallstones or heavy alcohol use. Most people with acute pancreatitis recover fully.
![]() Chronic Pancreatitis: This is a long-term inflammation of the pancreas that can lead to permanent damage. It often develops after an episode of acute pancreatitis or is caused by years of heavy alcohol use. Chronic pancreatitis can lead to digestive problems, diabetes, and chronic pain.
Chronic Pancreatitis: This is a long-term inflammation of the pancreas that can lead to permanent damage. It often develops after an episode of acute pancreatitis or is caused by years of heavy alcohol use. Chronic pancreatitis can lead to digestive problems, diabetes, and chronic pain.
Causes of Pancreatitis:
![]() Gallstones: Gallstones can block the bile duct or pancreatic duct, leading to a backup of enzymes.
Gallstones: Gallstones can block the bile duct or pancreatic duct, leading to a backup of enzymes.
![]() Alcohol Abuse: Excessive alcohol consumption is a major cause, particularly of chronic pancreatitis.
Alcohol Abuse: Excessive alcohol consumption is a major cause, particularly of chronic pancreatitis.
![]() High Triglyceride Levels: Very high levels of triglycerides in the blood can sometimes trigger pancreatitis.
High Triglyceride Levels: Very high levels of triglycerides in the blood can sometimes trigger pancreatitis.
![]() Certain Medications: Some medications have been linked to pancreatitis as a side effect (though this is less common).
Certain Medications: Some medications have been linked to pancreatitis as a side effect (though this is less common).
![]() Abdominal Injury: Trauma to the abdomen can sometimes cause pancreatitis.
Abdominal Injury: Trauma to the abdomen can sometimes cause pancreatitis.
![]() Infections: Some infections (e.g., mumps) can trigger pancreatitis.
Infections: Some infections (e.g., mumps) can trigger pancreatitis.
![]() Autoimmune Diseases: Conditions like lupus or Crohn's disease.
Autoimmune Diseases: Conditions like lupus or Crohn's disease.
![]() Cystic Fibrosis:
Cystic Fibrosis:
![]() Pancreatic Cancer: In rare cases
Pancreatic Cancer: In rare cases
![]() Idiopathic: In some cases, the cause is unknown (idiopathic pancreatitis).
Idiopathic: In some cases, the cause is unknown (idiopathic pancreatitis).
Symptoms of Pancreatitis:
![]() Acute Pancreatitis:
Acute Pancreatitis:![]()

![]() Severe abdominal pain (usually in the upper abdomen, often radiating to the back)
Severe abdominal pain (usually in the upper abdomen, often radiating to the back)![]()

![]() Nausea and vomiting
Nausea and vomiting![]()

![]() Fever
Fever![]()

![]() Rapid pulse
Rapid pulse![]()

![]() Swollen and tender abdomen
Swollen and tender abdomen
![]() Chronic Pancreatitis:
Chronic Pancreatitis:![]()

![]() Upper abdominal pain (which may be constant or intermittent)
Upper abdominal pain (which may be constant or intermittent)![]()

![]() Weight loss (due to malabsorption of nutrients)
Weight loss (due to malabsorption of nutrients)![]()

![]() Diarrhea
Diarrhea![]()

![]() Oily stools (steatorrhea)
Oily stools (steatorrhea)![]()

![]() Diabetes (in later stages)
Diabetes (in later stages)
Diagnosis:
Diagnosis typically involves:
![]() Physical Exam: A doctor will examine the abdomen and look for signs of tenderness and swelling.
Physical Exam: A doctor will examine the abdomen and look for signs of tenderness and swelling.
![]() Blood Tests: To check for elevated levels of pancreatic enzymes (amylase and lipase).
Blood Tests: To check for elevated levels of pancreatic enzymes (amylase and lipase).
![]() Imaging Tests:
Imaging Tests:![]()

![]() CT scan: Provides detailed images of the pancreas and surrounding organs.
CT scan: Provides detailed images of the pancreas and surrounding organs.![]()

![]() MRI: Another imaging technique that can show the pancreas and detect abnormalities.
MRI: Another imaging technique that can show the pancreas and detect abnormalities.![]()

![]() Ultrasound: Can be used to detect gallstones.
Ultrasound: Can be used to detect gallstones.![]()

![]() Endoscopic Ultrasound (EUS): A more invasive test where an ultrasound probe is attached to an endoscope (a thin, flexible tube) and inserted into the esophagus to get a closer look at the pancreas.
Endoscopic Ultrasound (EUS): A more invasive test where an ultrasound probe is attached to an endoscope (a thin, flexible tube) and inserted into the esophagus to get a closer look at the pancreas.
![]() Stool tests: May be done to check for fat malabsorption, especially in suspected chronic pancreatitis.
Stool tests: May be done to check for fat malabsorption, especially in suspected chronic pancreatitis.
Treatment:
Treatment depends on the type and severity of pancreatitis.
![]() Acute Pancreatitis:
Acute Pancreatitis:![]()

![]() Hospitalization: Usually required.
Hospitalization: Usually required.![]()

![]() IV Fluids: To prevent dehydration.
IV Fluids: To prevent dehydration.![]()

![]() Pain Medication: To manage pain.
Pain Medication: To manage pain.![]()

![]() NPO (Nothing by Mouth): To allow the pancreas to rest and recover. A feeding tube may be used if prolonged NPO is necessary.
NPO (Nothing by Mouth): To allow the pancreas to rest and recover. A feeding tube may be used if prolonged NPO is necessary.![]()

![]() Treatment of underlying cause: If gallstones are the cause, surgery (cholecystectomy) may be needed to remove the gallbladder.
Treatment of underlying cause: If gallstones are the cause, surgery (cholecystectomy) may be needed to remove the gallbladder.
![]() Chronic Pancreatitis:
Chronic Pancreatitis:![]()

![]() Pain Management: Can be challenging and may involve medications, nerve blocks, or surgery.
Pain Management: Can be challenging and may involve medications, nerve blocks, or surgery.![]()

![]() Pancreatic Enzyme Replacement Therapy (PERT): To help digest food and absorb nutrients.
Pancreatic Enzyme Replacement Therapy (PERT): To help digest food and absorb nutrients.![]()

![]() Dietary Changes: Low-fat diet, smaller meals, and avoidance of alcohol.
Dietary Changes: Low-fat diet, smaller meals, and avoidance of alcohol.![]()

![]() Diabetes Management: If diabetes develops.
Diabetes Management: If diabetes develops.![]()

![]() Surgery: In some cases, surgery may be needed to relieve blockages in the pancreatic duct or to remove damaged parts of the pancreas. Pancreatic islet cell transplantation is sometimes an option for those with severe pain.
Surgery: In some cases, surgery may be needed to relieve blockages in the pancreatic duct or to remove damaged parts of the pancreas. Pancreatic islet cell transplantation is sometimes an option for those with severe pain.![]()

![]() Lifestyle Changes: Abstinence from alcohol is crucial.
Lifestyle Changes: Abstinence from alcohol is crucial.
Complications:
Pancreatitis can lead to several complications, including:
![]() Pseudocysts: Fluid-filled sacs that can form on the pancreas.
Pseudocysts: Fluid-filled sacs that can form on the pancreas.
![]() Infection: Of the pancreas or surrounding tissues.
Infection: Of the pancreas or surrounding tissues.
![]() Kidney Failure
Kidney Failure
![]() Breathing Problems: Due to fluid buildup in the lungs.
Breathing Problems: Due to fluid buildup in the lungs.
![]() Diabetes: Especially in chronic pancreatitis, due to damage to the insulin-producing cells.
Diabetes: Especially in chronic pancreatitis, due to damage to the insulin-producing cells.
![]() Pancreatic Cancer: Chronic pancreatitis increases the risk of pancreatic cancer.
Pancreatic Cancer: Chronic pancreatitis increases the risk of pancreatic cancer.
![]() Malnutrition: Especially in chronic pancreatitis, due to impaired digestion and absorption.
Malnutrition: Especially in chronic pancreatitis, due to impaired digestion and absorption.
![]() Exocrine Pancreatic Insufficiency (EPI): The pancreas doesn't make enough enzymes to digest food properly.
Exocrine Pancreatic Insufficiency (EPI): The pancreas doesn't make enough enzymes to digest food properly.
Prevention:
![]() Avoid Excessive Alcohol Consumption: This is the most important preventive measure, particularly for chronic pancreatitis.
Avoid Excessive Alcohol Consumption: This is the most important preventive measure, particularly for chronic pancreatitis.
![]() Maintain a Healthy Weight: Obesity can increase the risk of gallstones.
Maintain a Healthy Weight: Obesity can increase the risk of gallstones.
![]() Eat a Healthy Diet: Low in fat and high in fiber.
Eat a Healthy Diet: Low in fat and high in fiber.
![]() Get Regular Exercise:
Get Regular Exercise:
![]() If you have gallstones, discuss treatment options with your doctor.
If you have gallstones, discuss treatment options with your doctor.
Important Note: This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment. Self-treating can be dangerous. If you suspect you have pancreatitis, seek immediate medical attention.