Pericarditis
Published: 18 Jun 2025
ICD9: 420.90 ICD10: I30.9 ICD11: BB20
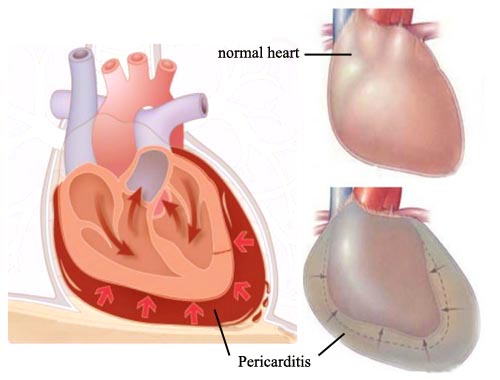
Pericarditis is an inflammation of the pericardium, the thin, sac-like membrane surrounding the heart.
Think of it as an irritation of the "bag" that holds your heart.
Here's a breakdown:
![]() Pericardium: This is a double-layered sac that surrounds the heart. The layers are:
Pericardium: This is a double-layered sac that surrounds the heart. The layers are:![]()

![]() Visceral pericardium: The inner layer, directly attached to the heart.
Visceral pericardium: The inner layer, directly attached to the heart.![]()

![]() Parietal pericardium: The outer layer.
Parietal pericardium: The outer layer.![]()

![]() Pericardial space: The space between these layers contains a small amount of fluid (pericardial fluid) that helps lubricate the heart as it beats, reducing friction.
Pericardial space: The space between these layers contains a small amount of fluid (pericardial fluid) that helps lubricate the heart as it beats, reducing friction.
![]() Inflammation: When the pericardium becomes inflamed, it can cause various problems.
Inflammation: When the pericardium becomes inflamed, it can cause various problems.
Causes:
Many things can cause pericarditis, including:
![]() Viral infections: This is the most common cause (e.g., Coxsackievirus, Echovirus).
Viral infections: This is the most common cause (e.g., Coxsackievirus, Echovirus).
![]() Bacterial infections: Less common than viral, but can be serious.
Bacterial infections: Less common than viral, but can be serious.
![]() Fungal infections: Rare.
Fungal infections: Rare.
![]() Autoimmune diseases: (e.g., lupus, rheumatoid arthritis).
Autoimmune diseases: (e.g., lupus, rheumatoid arthritis).
![]() Heart attack: Pericarditis can occur after a heart attack (Dressler's syndrome).
Heart attack: Pericarditis can occur after a heart attack (Dressler's syndrome).
![]() Heart surgery:
Heart surgery:
![]() Trauma: Injury to the chest.
Trauma: Injury to the chest.
![]() Kidney failure:
Kidney failure:
![]() Cancer:
Cancer:
![]() Certain medications:
Certain medications:
![]() Idiopathic: Sometimes, the cause is unknown.
Idiopathic: Sometimes, the cause is unknown.
Symptoms:
![]() Chest pain: This is the most common symptom. It's often:
Chest pain: This is the most common symptom. It's often:![]()

![]() Sharp, stabbing pain.
Sharp, stabbing pain.![]()

![]() Located in the center or left side of the chest.
Located in the center or left side of the chest.![]()

![]() Worse with breathing, coughing, or lying down.
Worse with breathing, coughing, or lying down.![]()

![]() Relieved by sitting up and leaning forward.
Relieved by sitting up and leaning forward.
![]() Shortness of breath
Shortness of breath
![]() Palpitations (irregular heartbeats)
Palpitations (irregular heartbeats)
![]() Fatigue
Fatigue
![]() Low-grade fever
Low-grade fever
![]() Cough
Cough
![]() Swelling in the legs and ankles
Swelling in the legs and ankles
Complications:
![]() Pericardial effusion: An excessive buildup of fluid in the pericardial sac.
Pericardial effusion: An excessive buildup of fluid in the pericardial sac.
![]() Cardiac tamponade: A life-threatening condition where the buildup of fluid in the pericardial sac compresses the heart, preventing it from pumping effectively.
Cardiac tamponade: A life-threatening condition where the buildup of fluid in the pericardial sac compresses the heart, preventing it from pumping effectively.
![]() Constrictive pericarditis: A chronic condition where the pericardium becomes thickened and scarred, restricting the heart's ability to expand and fill with blood.
Constrictive pericarditis: A chronic condition where the pericardium becomes thickened and scarred, restricting the heart's ability to expand and fill with blood.
Diagnosis:
![]() Physical exam: Listening to the heart with a stethoscope can reveal a characteristic "pericardial friction rub" sound.
Physical exam: Listening to the heart with a stethoscope can reveal a characteristic "pericardial friction rub" sound.
![]() Electrocardiogram (ECG or EKG): Can show specific changes associated with pericarditis.
Electrocardiogram (ECG or EKG): Can show specific changes associated with pericarditis.
![]() Echocardiogram: An ultrasound of the heart to assess its structure and function, and to look for pericardial effusion.
Echocardiogram: An ultrasound of the heart to assess its structure and function, and to look for pericardial effusion.
![]() Chest X-ray: To evaluate the size and shape of the heart and look for signs of fluid.
Chest X-ray: To evaluate the size and shape of the heart and look for signs of fluid.
![]() Blood tests: To look for signs of infection, inflammation, or kidney problems.
Blood tests: To look for signs of infection, inflammation, or kidney problems.
Treatment:
Treatment depends on the cause and severity of the pericarditis:
![]() Pain relievers: NSAIDs (nonsteroidal anti-inflammatory drugs) like ibuprofen or aspirin are often used to reduce pain and inflammation.
Pain relievers: NSAIDs (nonsteroidal anti-inflammatory drugs) like ibuprofen or aspirin are often used to reduce pain and inflammation.
![]() Colchicine: An anti-inflammatory drug that is often used in addition to NSAIDs.
Colchicine: An anti-inflammatory drug that is often used in addition to NSAIDs.
![]() Corticosteroids: May be used if NSAIDs and colchicine are not effective or are contraindicated.
Corticosteroids: May be used if NSAIDs and colchicine are not effective or are contraindicated.
![]() Antibiotics, antifungals, or antiviral medications: If the pericarditis is caused by an infection.
Antibiotics, antifungals, or antiviral medications: If the pericarditis is caused by an infection.
![]() Pericardiocentesis: A procedure to drain excess fluid from the pericardial sac, especially in cases of cardiac tamponade.
Pericardiocentesis: A procedure to drain excess fluid from the pericardial sac, especially in cases of cardiac tamponade.
![]() Pericardiectomy: Surgical removal of the pericardium, usually for constrictive pericarditis.
Pericardiectomy: Surgical removal of the pericardium, usually for constrictive pericarditis.
In summary: Pericarditis is inflammation of the sac surrounding the heart, causing chest pain and potentially serious complications. Diagnosis involves physical exam, ECG, and other tests, and treatment aims to reduce inflammation and manage symptoms. It's essential to seek medical attention if you experience chest pain, especially if it's accompanied by other symptoms like shortness of breath or fever.