Polycystic Ovary syndrome, PCOS
Published: 18 Jun 2025
ICD9: 256.4 ICD10: E28.2 ICD11: 5A80.1
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age.
It's characterized by imbalances in reproductive hormones, which can lead to a variety of symptoms and health problems. The exact cause of PCOS is unknown, but it's believed to be a combination of genetic and environmental factors.
Here's a breakdown of key aspects of PCOS:
Key Features and Diagnostic Criteria:
Typically, a diagnosis of PCOS involves having at least two out of the following three features (Rotterdam criteria):
![]() Irregular or Absent Periods: This is often the most noticeable symptom. Women with PCOS may have infrequent, irregular, prolonged, or absent menstrual cycles. This irregularity is due to irregular ovulation or a lack of ovulation (anovulation).
Irregular or Absent Periods: This is often the most noticeable symptom. Women with PCOS may have infrequent, irregular, prolonged, or absent menstrual cycles. This irregularity is due to irregular ovulation or a lack of ovulation (anovulation).
![]() Excess Androgens (Hyperandrogenism): Androgens are often called "male hormones" because they are present at higher levels in men, but women produce them too. In PCOS, women may have elevated levels of androgens in their blood or have physical signs of excess androgens, such as:
Excess Androgens (Hyperandrogenism): Androgens are often called "male hormones" because they are present at higher levels in men, but women produce them too. In PCOS, women may have elevated levels of androgens in their blood or have physical signs of excess androgens, such as:![]()

![]() Hirsutism: Excessive hair growth on the face, chest, back, or abdomen.
Hirsutism: Excessive hair growth on the face, chest, back, or abdomen.![]()

![]() Acne: Persistent or severe acne, often resistant to typical treatments.
Acne: Persistent or severe acne, often resistant to typical treatments.![]()

![]() Alopecia (Male-pattern Baldness): Thinning hair on the scalp, particularly around the hairline.
Alopecia (Male-pattern Baldness): Thinning hair on the scalp, particularly around the hairline.
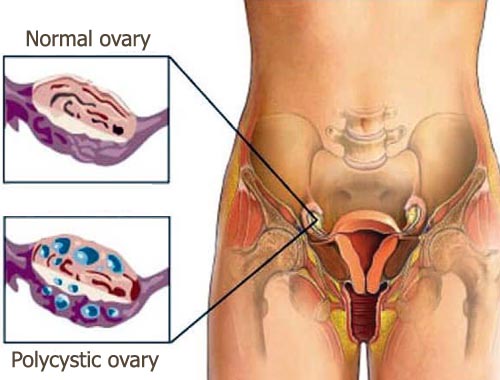
![]() Polycystic Ovaries: An ultrasound may show that the ovaries are enlarged and contain numerous small follicles (fluid-filled sacs) that surround the eggs. However, it's important to note that:
Polycystic Ovaries: An ultrasound may show that the ovaries are enlarged and contain numerous small follicles (fluid-filled sacs) that surround the eggs. However, it's important to note that:![]()

![]() Having polycystic ovaries alone does *not* mean you have PCOS. Many women have them without any other symptoms.
Having polycystic ovaries alone does *not* mean you have PCOS. Many women have them without any other symptoms.![]()

![]() Conversely, you can have PCOS without having polycystic ovaries detected on ultrasound.
Conversely, you can have PCOS without having polycystic ovaries detected on ultrasound.
Other Common Symptoms and Associated Health Problems:
Besides the core diagnostic criteria, women with PCOS may experience:
![]() Infertility: Due to irregular or absent ovulation, PCOS is a leading cause of infertility.
Infertility: Due to irregular or absent ovulation, PCOS is a leading cause of infertility.
![]() Weight Gain or Difficulty Losing Weight: Many women with PCOS struggle with weight management, and are prone to weight gain, especially around the abdomen.
Weight Gain or Difficulty Losing Weight: Many women with PCOS struggle with weight management, and are prone to weight gain, especially around the abdomen.
![]() Insulin Resistance: This means the body doesn't respond properly to insulin, a hormone that regulates blood sugar. Insulin resistance can lead to:
Insulin Resistance: This means the body doesn't respond properly to insulin, a hormone that regulates blood sugar. Insulin resistance can lead to:![]()

![]() High Blood Sugar (Hyperglycemia): Increasing the risk of prediabetes and type 2 diabetes.
High Blood Sugar (Hyperglycemia): Increasing the risk of prediabetes and type 2 diabetes.![]()

![]() Acanthosis Nigricans: Dark, velvety patches of skin, often in the armpits, groin, or neck.
Acanthosis Nigricans: Dark, velvety patches of skin, often in the armpits, groin, or neck.
![]() Increased Risk of Metabolic Syndrome: A cluster of conditions including high blood pressure, high blood sugar, abnormal cholesterol levels, and excess abdominal fat, increasing the risk of heart disease, stroke, and diabetes.
Increased Risk of Metabolic Syndrome: A cluster of conditions including high blood pressure, high blood sugar, abnormal cholesterol levels, and excess abdominal fat, increasing the risk of heart disease, stroke, and diabetes.
![]() Sleep Apnea: A sleep disorder where breathing repeatedly stops and starts during the night.
Sleep Apnea: A sleep disorder where breathing repeatedly stops and starts during the night.
![]() Anxiety and Depression: PCOS can contribute to mood disorders.
Anxiety and Depression: PCOS can contribute to mood disorders.
![]() Endometrial Cancer: Irregular periods can lead to a thickening of the uterine lining (endometrium), increasing the risk of endometrial cancer if left unmanaged.
Endometrial Cancer: Irregular periods can lead to a thickening of the uterine lining (endometrium), increasing the risk of endometrial cancer if left unmanaged.
Diagnosis:
Diagnosing PCOS usually involves:
![]() Medical History and Physical Exam: The doctor will ask about your menstrual cycles, symptoms, and medical history.
Medical History and Physical Exam: The doctor will ask about your menstrual cycles, symptoms, and medical history.
![]() Pelvic Exam: To assess the reproductive organs.
Pelvic Exam: To assess the reproductive organs.
![]() Blood Tests: To measure hormone levels (androgens, insulin, glucose), cholesterol levels, and other indicators.
Blood Tests: To measure hormone levels (androgens, insulin, glucose), cholesterol levels, and other indicators.
![]() Ultrasound: To visualize the ovaries and uterus.
Ultrasound: To visualize the ovaries and uterus.
Treatment:
There is no cure for PCOS, but the symptoms can be managed effectively with lifestyle changes and medications. Treatment options depend on the specific symptoms and concerns of the individual:
![]() Lifestyle Modifications:
Lifestyle Modifications:![]()

![]() Weight Management: Losing even a small amount of weight can significantly improve PCOS symptoms and reduce the risk of complications. A healthy diet and regular exercise are crucial.
Weight Management: Losing even a small amount of weight can significantly improve PCOS symptoms and reduce the risk of complications. A healthy diet and regular exercise are crucial.![]()

![]() Diet: Focusing on a balanced diet rich in fruits, vegetables, whole grains, and lean protein. Limiting processed foods, sugary drinks, and unhealthy fats.
Diet: Focusing on a balanced diet rich in fruits, vegetables, whole grains, and lean protein. Limiting processed foods, sugary drinks, and unhealthy fats.![]()

![]() Exercise: Regular physical activity improves insulin sensitivity, helps with weight management, and can improve mood.
Exercise: Regular physical activity improves insulin sensitivity, helps with weight management, and can improve mood.
![]() Medications:
Medications:![]()

![]() Birth Control Pills: To regulate menstrual cycles, reduce androgen levels, and treat acne and hirsutism.
Birth Control Pills: To regulate menstrual cycles, reduce androgen levels, and treat acne and hirsutism.![]()

![]() Metformin: A medication commonly used to treat type 2 diabetes. It improves insulin sensitivity and can help regulate menstrual cycles and ovulation.
Metformin: A medication commonly used to treat type 2 diabetes. It improves insulin sensitivity and can help regulate menstrual cycles and ovulation.![]()

![]() Anti-Androgens: Medications that block the effects of androgens, such as spironolactone. They can help treat hirsutism and acne.
Anti-Androgens: Medications that block the effects of androgens, such as spironolactone. They can help treat hirsutism and acne.![]()

![]() Fertility Treatments: Medications like clomiphene or letrozole, or procedures like in vitro fertilization (IVF), to help with ovulation and increase the chances of pregnancy.
Fertility Treatments: Medications like clomiphene or letrozole, or procedures like in vitro fertilization (IVF), to help with ovulation and increase the chances of pregnancy.![]()

![]() Progestin Therapy: To induce regular periods and prevent endometrial hyperplasia (thickening of the uterine lining) in women who don't ovulate regularly.
Progestin Therapy: To induce regular periods and prevent endometrial hyperplasia (thickening of the uterine lining) in women who don't ovulate regularly.
Important Considerations:
![]() Individualized Treatment: PCOS affects each woman differently, so treatment plans should be tailored to individual needs and goals.
Individualized Treatment: PCOS affects each woman differently, so treatment plans should be tailored to individual needs and goals.
![]() Long-Term Management: PCOS is a chronic condition, so ongoing management is important to prevent long-term health complications.
Long-Term Management: PCOS is a chronic condition, so ongoing management is important to prevent long-term health complications.
![]() Consultation with a Specialist: It's essential to consult with a doctor, preferably an endocrinologist or a gynecologist specializing in reproductive endocrinology, for proper diagnosis and management of PCOS.
Consultation with a Specialist: It's essential to consult with a doctor, preferably an endocrinologist or a gynecologist specializing in reproductive endocrinology, for proper diagnosis and management of PCOS.
It is important to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan. This information is not intended as a substitute for professional medical advice.