Primary Sclerosing Cholangitis
Published: 18 Jun 2025
ICD9: 576.1 ICD10: K83.0 ICD11: DB96.2
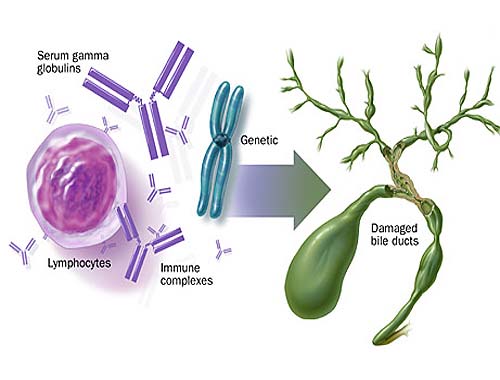
Primary Sclerosing Cholangitis (PSC) is a chronic liver disease characterized by inflammation and scarring (sclerosis) of the bile ducts inside and outside the liver.
These ducts are tubes that carry bile from the liver to the gallbladder and small intestine, where it helps with digestion.
Here's a breakdown of key aspects of PSC:
![]() Inflammation and Scarring: PSC causes inflammation within the bile ducts, leading to their gradual scarring. This scarring narrows the ducts, obstructing the flow of bile.
Inflammation and Scarring: PSC causes inflammation within the bile ducts, leading to their gradual scarring. This scarring narrows the ducts, obstructing the flow of bile.
![]() Bile Buildup: As the bile ducts narrow and block, bile begins to accumulate in the liver. This buildup can damage liver cells.
Bile Buildup: As the bile ducts narrow and block, bile begins to accumulate in the liver. This buildup can damage liver cells.
![]() Progressive Damage: PSC is a progressive disease, meaning it worsens over time. The continued inflammation and scarring eventually lead to cirrhosis (severe scarring of the liver), liver failure, and other complications.
Progressive Damage: PSC is a progressive disease, meaning it worsens over time. The continued inflammation and scarring eventually lead to cirrhosis (severe scarring of the liver), liver failure, and other complications.
![]() Cause: The exact cause of PSC is unknown. It is considered an autoimmune disease, meaning the body's immune system mistakenly attacks the bile ducts. Genetics may play a role, as people with certain gene variations are more likely to develop PSC. It's frequently associated with inflammatory bowel disease (IBD), particularly ulcerative colitis.
Cause: The exact cause of PSC is unknown. It is considered an autoimmune disease, meaning the body's immune system mistakenly attacks the bile ducts. Genetics may play a role, as people with certain gene variations are more likely to develop PSC. It's frequently associated with inflammatory bowel disease (IBD), particularly ulcerative colitis.
![]() Symptoms: Many people with PSC have no symptoms, especially in the early stages. When symptoms do appear, they can include:
Symptoms: Many people with PSC have no symptoms, especially in the early stages. When symptoms do appear, they can include:![]()

![]() Fatigue
Fatigue![]()

![]() Itching (pruritus)
Itching (pruritus)![]()

![]() Jaundice (yellowing of the skin and eyes)
Jaundice (yellowing of the skin and eyes)![]()

![]() Abdominal pain
Abdominal pain![]()

![]() Fever
Fever![]()

![]() Night sweats
Night sweats![]()

![]() Weight loss
Weight loss![]()

![]() Enlarged liver or spleen
Enlarged liver or spleen
![]() Diagnosis: PSC is usually diagnosed through a combination of:
Diagnosis: PSC is usually diagnosed through a combination of:![]()

![]() Liver function tests: Blood tests that assess how well the liver is functioning.
Liver function tests: Blood tests that assess how well the liver is functioning.![]()

![]() Imaging tests:
Imaging tests:![]()

![]() Magnetic Resonance Cholangiopancreatography (MRCP): An MRI scan that specifically visualizes the bile ducts. This is the primary diagnostic test.
Magnetic Resonance Cholangiopancreatography (MRCP): An MRI scan that specifically visualizes the bile ducts. This is the primary diagnostic test.![]()

![]() Endoscopic Retrograde Cholangiopancreatography (ERCP): A more invasive procedure where a scope is inserted down the throat to visualize the bile ducts. It can also be used to take biopsies or place stents.
Endoscopic Retrograde Cholangiopancreatography (ERCP): A more invasive procedure where a scope is inserted down the throat to visualize the bile ducts. It can also be used to take biopsies or place stents.![]()

![]() Liver biopsy: A small sample of liver tissue is taken for examination under a microscope. This is not always necessary for diagnosis, but can help determine the severity of the disease.
Liver biopsy: A small sample of liver tissue is taken for examination under a microscope. This is not always necessary for diagnosis, but can help determine the severity of the disease.
![]() Complications: PSC can lead to various complications, including:
Complications: PSC can lead to various complications, including:![]()

![]() Cirrhosis: Severe scarring of the liver.
Cirrhosis: Severe scarring of the liver.![]()

![]() Liver failure: The liver is unable to function properly.
Liver failure: The liver is unable to function properly.![]()

![]() Cholangiocarcinoma: Cancer of the bile ducts. People with PSC have a higher risk of developing this type of cancer.
Cholangiocarcinoma: Cancer of the bile ducts. People with PSC have a higher risk of developing this type of cancer.![]()

![]() Colon cancer: Increased risk, especially in those with IBD.
Colon cancer: Increased risk, especially in those with IBD.![]()

![]() Infections: Bile duct infections (cholangitis).
Infections: Bile duct infections (cholangitis).![]()

![]() Portal hypertension: High blood pressure in the portal vein, which carries blood from the intestines to the liver.
Portal hypertension: High blood pressure in the portal vein, which carries blood from the intestines to the liver.![]()

![]() Varices: Enlarged veins in the esophagus or stomach that can bleed.
Varices: Enlarged veins in the esophagus or stomach that can bleed.
![]() Treatment: There is no cure for PSC. Treatment focuses on managing symptoms, slowing the progression of the disease, and preventing complications. Treatment options include:
Treatment: There is no cure for PSC. Treatment focuses on managing symptoms, slowing the progression of the disease, and preventing complications. Treatment options include:![]()

![]() Medications:
Medications:![]()

![]() Ursodeoxycholic acid (UDCA): A bile acid that may help improve liver function.
Ursodeoxycholic acid (UDCA): A bile acid that may help improve liver function.![]()

![]() Medications to relieve itching: Cholestyramine, rifampin, or naltrexone.
Medications to relieve itching: Cholestyramine, rifampin, or naltrexone.![]()

![]() Antibiotics: To treat bile duct infections.
Antibiotics: To treat bile duct infections.![]()

![]() Endoscopic procedures: ERCP to dilate narrowed bile ducts or place stents to keep them open.
Endoscopic procedures: ERCP to dilate narrowed bile ducts or place stents to keep them open.![]()

![]() Liver transplant: For people with advanced liver disease or complications of PSC, a liver transplant may be the only option.
Liver transplant: For people with advanced liver disease or complications of PSC, a liver transplant may be the only option.![]()

![]() Regular monitoring: Surveillance for complications such as cholangiocarcinoma and colon cancer is essential.
Regular monitoring: Surveillance for complications such as cholangiocarcinoma and colon cancer is essential.
![]() Prognosis: The prognosis for people with PSC varies. Some people may live for many years with minimal symptoms, while others may experience a more rapid progression of the disease. Liver transplant can improve survival for those with advanced disease.
Prognosis: The prognosis for people with PSC varies. Some people may live for many years with minimal symptoms, while others may experience a more rapid progression of the disease. Liver transplant can improve survival for those with advanced disease.
Important Considerations:
![]() PSC is a rare disease.
PSC is a rare disease.
![]() It's important to seek care from a gastroenterologist or hepatologist (liver specialist) experienced in managing PSC.
It's important to seek care from a gastroenterologist or hepatologist (liver specialist) experienced in managing PSC.
![]() Because of the link with IBD, people with PSC should also be monitored for IBD.
Because of the link with IBD, people with PSC should also be monitored for IBD.
Disclaimer: This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.