Prosthetic Heart Valve Hemolysis
Published: 18 Jun 2025
ICD9: 429.4 ICD10: I97.130 ICD11: QB50.2
Prosthetic heart valve hemolysis is a condition where red blood cells (RBCs) are damaged and destroyed (hemolyzed) as they flow through or around a prosthetic (artificial) heart valve.
This destruction of RBCs releases their contents into the bloodstream, leading to anemia and other complications.
Here's a breakdown of the key aspects:
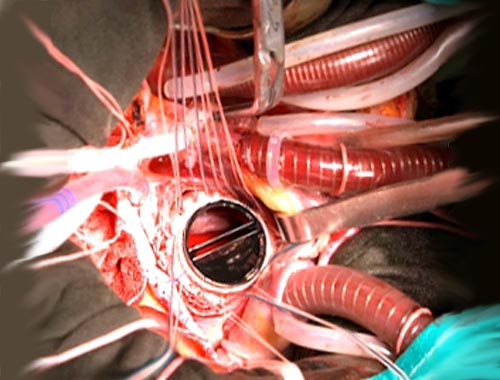
![]() Prosthetic Heart Valve: This refers to an artificial valve implanted in the heart to replace a diseased or damaged natural valve.
Prosthetic Heart Valve: This refers to an artificial valve implanted in the heart to replace a diseased or damaged natural valve.
![]() Hemolysis: This is the destruction of red blood cells. When RBCs break down, they release hemoglobin (the oxygen-carrying protein) into the plasma.
Hemolysis: This is the destruction of red blood cells. When RBCs break down, they release hemoglobin (the oxygen-carrying protein) into the plasma.
![]() Mechanism: The damage to RBCs typically happens due to:
Mechanism: The damage to RBCs typically happens due to:![]()

![]() High Shear Stress: Blood flowing at high velocity and turbulence, often occurring around the valve leaflets or sewing ring (the part that attaches the valve to the heart), can physically damage the RBCs.
High Shear Stress: Blood flowing at high velocity and turbulence, often occurring around the valve leaflets or sewing ring (the part that attaches the valve to the heart), can physically damage the RBCs.![]()

![]() Mechanical Trauma: Direct contact or impact with the valve structure can also cause RBC damage.
Mechanical Trauma: Direct contact or impact with the valve structure can also cause RBC damage.![]()

![]() Paravalvular Leak: A leak around the valve (paravalvular leak) can create high-velocity jets of blood that damage RBCs.
Paravalvular Leak: A leak around the valve (paravalvular leak) can create high-velocity jets of blood that damage RBCs.![]()

![]() Valve Stenosis: Narrowing of the valve opening can also increase blood flow velocity and turbulence leading to RBC damage.
Valve Stenosis: Narrowing of the valve opening can also increase blood flow velocity and turbulence leading to RBC damage.
Consequences of Prosthetic Heart Valve Hemolysis:
![]() Anemia: The most direct consequence. The destruction of RBCs leads to a lower than normal red blood cell count, causing fatigue, weakness, and shortness of breath.
Anemia: The most direct consequence. The destruction of RBCs leads to a lower than normal red blood cell count, causing fatigue, weakness, and shortness of breath.
![]() Elevated LDH (Lactate Dehydrogenase): LDH is an enzyme released from damaged cells, including RBCs. An elevated LDH level is a common indicator of hemolysis.
Elevated LDH (Lactate Dehydrogenase): LDH is an enzyme released from damaged cells, including RBCs. An elevated LDH level is a common indicator of hemolysis.
![]() Elevated Bilirubin: Hemoglobin breaks down into bilirubin. Increased hemolysis can lead to elevated bilirubin levels, sometimes causing jaundice (yellowing of the skin and eyes).
Elevated Bilirubin: Hemoglobin breaks down into bilirubin. Increased hemolysis can lead to elevated bilirubin levels, sometimes causing jaundice (yellowing of the skin and eyes).
![]() Decreased Haptoglobin: Haptoglobin is a protein that binds to free hemoglobin in the blood. When hemolysis occurs, haptoglobin is used up quickly, leading to decreased levels.
Decreased Haptoglobin: Haptoglobin is a protein that binds to free hemoglobin in the blood. When hemolysis occurs, haptoglobin is used up quickly, leading to decreased levels.
![]() Hemoglobinuria: In severe cases, hemoglobin can be present in the urine, giving it a reddish or brownish color.
Hemoglobinuria: In severe cases, hemoglobin can be present in the urine, giving it a reddish or brownish color.
![]() Iron Deficiency: Chronic hemolysis can lead to iron loss, contributing to iron deficiency anemia.
Iron Deficiency: Chronic hemolysis can lead to iron loss, contributing to iron deficiency anemia.
![]() Renal (Kidney) Damage: In rare cases, the release of hemoglobin into the bloodstream can overwhelm the kidneys, leading to acute kidney injury.
Renal (Kidney) Damage: In rare cases, the release of hemoglobin into the bloodstream can overwhelm the kidneys, leading to acute kidney injury.
![]() Thrombosis (Blood Clots): Hemolysis can, paradoxically, increase the risk of blood clot formation in some situations.
Thrombosis (Blood Clots): Hemolysis can, paradoxically, increase the risk of blood clot formation in some situations.
Diagnosis:
Diagnosing prosthetic valve hemolysis involves:
![]() Blood Tests: Complete blood count (CBC) to assess red blood cell count and indices, LDH, bilirubin, haptoglobin, reticulocyte count (immature red blood cells), and iron studies.
Blood Tests: Complete blood count (CBC) to assess red blood cell count and indices, LDH, bilirubin, haptoglobin, reticulocyte count (immature red blood cells), and iron studies.
![]() Urine Analysis: To check for hemoglobinuria.
Urine Analysis: To check for hemoglobinuria.
![]() Echocardiogram: To evaluate valve function, assess for paravalvular leaks, and measure pressure gradients across the valve.
Echocardiogram: To evaluate valve function, assess for paravalvular leaks, and measure pressure gradients across the valve.
![]() Cardiac Catheterization: In some cases, this might be needed for more detailed assessment of valve function and pressures.
Cardiac Catheterization: In some cases, this might be needed for more detailed assessment of valve function and pressures.
Treatment:
Treatment depends on the severity of the hemolysis:
![]() Mild Hemolysis: May require observation and iron supplementation.
Mild Hemolysis: May require observation and iron supplementation.
![]() Moderate to Severe Hemolysis:
Moderate to Severe Hemolysis:![]()

![]() Medications: Erythropoietin-stimulating agents (ESAs) may be used to stimulate red blood cell production.
Medications: Erythropoietin-stimulating agents (ESAs) may be used to stimulate red blood cell production.![]()

![]() Blood Transfusions: To replenish red blood cells in severe anemia.
Blood Transfusions: To replenish red blood cells in severe anemia.![]()

![]() Surgery or Intervention: If a paravalvular leak or valve dysfunction is causing the hemolysis, surgery or a percutaneous intervention (e.g., using a catheter to close the leak) may be necessary to repair or replace the valve.
Surgery or Intervention: If a paravalvular leak or valve dysfunction is causing the hemolysis, surgery or a percutaneous intervention (e.g., using a catheter to close the leak) may be necessary to repair or replace the valve.
Important Considerations:
![]() Some degree of hemolysis can be normal in patients with prosthetic heart valves, but significant hemolysis causing anemia or other complications requires investigation and treatment.
Some degree of hemolysis can be normal in patients with prosthetic heart valves, but significant hemolysis causing anemia or other complications requires investigation and treatment.
![]() The risk of hemolysis varies depending on the type, size, and position of the valve, as well as individual patient factors.
The risk of hemolysis varies depending on the type, size, and position of the valve, as well as individual patient factors.
![]() Regular monitoring with blood tests and echocardiograms is essential for patients with prosthetic heart valves.
Regular monitoring with blood tests and echocardiograms is essential for patients with prosthetic heart valves.
This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.