Pulmonary Edema (Fluid in the Lungs)
Published: 18 Jun 2025
ICD9: 518.4 ICD10: J81.0 ICD11: CB01
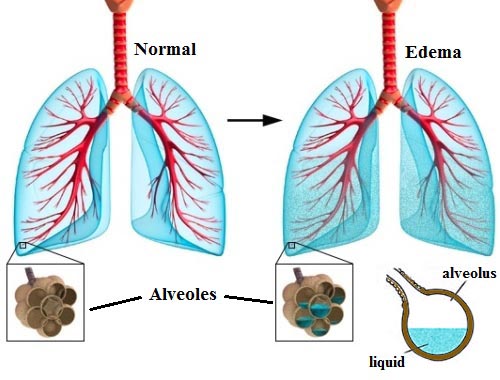
Pulmonary edema is a condition where excess fluid accumulates in the lungs, specifically in the air sacs (alveoli).
This fluid interferes with normal gas exchange, making it difficult to breathe and can be life-threatening if left untreated.
Think of your lungs like a sponge. Normally, the sponge is filled with air. In pulmonary edema, the sponge gets filled with water, making it hard for air to get in and out.
Here's a breakdown of key aspects of pulmonary edema:
Causes:
![]() Heart problems (Cardiogenic Pulmonary Edema): This is the most common cause. When the heart can't pump blood effectively, pressure builds up in the blood vessels in the lungs, forcing fluid into the alveoli. Common heart conditions leading to this include:
Heart problems (Cardiogenic Pulmonary Edema): This is the most common cause. When the heart can't pump blood effectively, pressure builds up in the blood vessels in the lungs, forcing fluid into the alveoli. Common heart conditions leading to this include:![]()

![]() Congestive heart failure
Congestive heart failure![]()

![]() Coronary artery disease
Coronary artery disease![]()

![]() Heart valve problems
Heart valve problems![]()

![]() High blood pressure
High blood pressure![]()

![]() Cardiomyopathy
Cardiomyopathy
![]() Non-heart problems (Non-Cardiogenic Pulmonary Edema): In this case, the heart is working fine, but there's damage to the lungs or other issues causing the fluid to leak into the alveoli. Examples include:
Non-heart problems (Non-Cardiogenic Pulmonary Edema): In this case, the heart is working fine, but there's damage to the lungs or other issues causing the fluid to leak into the alveoli. Examples include:![]()

![]() Acute Respiratory Distress Syndrome (ARDS): A severe lung condition caused by infections, trauma, or other lung injuries.
Acute Respiratory Distress Syndrome (ARDS): A severe lung condition caused by infections, trauma, or other lung injuries.![]()

![]() Kidney failure: Kidneys not removing enough fluid can overload the body and cause fluid to back up into the lungs.
Kidney failure: Kidneys not removing enough fluid can overload the body and cause fluid to back up into the lungs.![]()

![]() High altitude pulmonary edema (HAPE): Occurs in people traveling to high altitudes due to changes in lung pressure.
High altitude pulmonary edema (HAPE): Occurs in people traveling to high altitudes due to changes in lung pressure.![]()

![]() Near drowning: Inhaling water damages the lungs.
Near drowning: Inhaling water damages the lungs.![]()

![]() Lung infections (pneumonia): Inflammation and fluid accumulation can occur.
Lung infections (pneumonia): Inflammation and fluid accumulation can occur.![]()

![]() Toxic gas inhalation: Damage to the lung tissue.
Toxic gas inhalation: Damage to the lung tissue.![]()

![]() Drug overdose: Certain drugs can damage the lungs.
Drug overdose: Certain drugs can damage the lungs.![]()

![]() Blood clots in the lungs (pulmonary embolism): Disrupts blood flow and can lead to edema.
Blood clots in the lungs (pulmonary embolism): Disrupts blood flow and can lead to edema.![]()

![]() Severe infection (sepsis): Can cause widespread inflammation and lung damage.
Severe infection (sepsis): Can cause widespread inflammation and lung damage.![]()

![]() Transfusion-related acute lung injury (TRALI): A rare but serious complication of blood transfusions.
Transfusion-related acute lung injury (TRALI): A rare but serious complication of blood transfusions.
Symptoms:
Symptoms can vary depending on the severity and how quickly the edema develops.
![]() Sudden (Acute) Pulmonary Edema: This is a medical emergency.
Sudden (Acute) Pulmonary Edema: This is a medical emergency.![]()

![]() Extreme shortness of breath or difficulty breathing (dyspnea)
Extreme shortness of breath or difficulty breathing (dyspnea)![]()

![]() Gasping for air
Gasping for air![]()

![]() Wheezing or gurgling sounds (rales or crackles)
Wheezing or gurgling sounds (rales or crackles)![]()

![]() Coughing up frothy, blood-tinged sputum (pink and foamy)
Coughing up frothy, blood-tinged sputum (pink and foamy)![]()

![]() Rapid heartbeat
Rapid heartbeat![]()

![]() Anxiety, restlessness, or sense of suffocation
Anxiety, restlessness, or sense of suffocation![]()

![]() Bluish skin color (cyanosis) due to lack of oxygen
Bluish skin color (cyanosis) due to lack of oxygen![]()

![]() Sweating
Sweating![]()

![]() Chest pain (if related to heart problems)
Chest pain (if related to heart problems)
![]() Gradual (Chronic) Pulmonary Edema: Symptoms develop slowly over time.
Gradual (Chronic) Pulmonary Edema: Symptoms develop slowly over time.![]()

![]() Shortness of breath with exertion (getting tired easily)
Shortness of breath with exertion (getting tired easily)![]()

![]() Difficulty breathing when lying down (orthopnea) - requires propping up with pillows
Difficulty breathing when lying down (orthopnea) - requires propping up with pillows![]()

![]() Nighttime shortness of breath that wakes you up (paroxysmal nocturnal dyspnea)
Nighttime shortness of breath that wakes you up (paroxysmal nocturnal dyspnea)![]()

![]() Swelling in the legs and feet (edema)
Swelling in the legs and feet (edema)![]()

![]() Weight gain
Weight gain
Diagnosis:
![]() Physical Exam: Listening to the lungs with a stethoscope can reveal crackling sounds (rales).
Physical Exam: Listening to the lungs with a stethoscope can reveal crackling sounds (rales).
![]() Chest X-ray: Shows fluid in the lungs and can help identify the cause (e.g., enlarged heart).
Chest X-ray: Shows fluid in the lungs and can help identify the cause (e.g., enlarged heart).
![]() Blood tests: To check oxygen and carbon dioxide levels, kidney function, and look for markers of heart damage (e.g., BNP).
Blood tests: To check oxygen and carbon dioxide levels, kidney function, and look for markers of heart damage (e.g., BNP).
![]() Electrocardiogram (ECG/EKG): To assess heart rhythm and look for signs of heart attack or other heart problems.
Electrocardiogram (ECG/EKG): To assess heart rhythm and look for signs of heart attack or other heart problems.
![]() Echocardiogram: Ultrasound of the heart to assess its pumping function and valve function.
Echocardiogram: Ultrasound of the heart to assess its pumping function and valve function.
![]() Pulse oximetry: Measures oxygen saturation in the blood.
Pulse oximetry: Measures oxygen saturation in the blood.
![]() Arterial blood gas (ABG): Measures the levels of oxygen and carbon dioxide in the blood, as well as the pH.
Arterial blood gas (ABG): Measures the levels of oxygen and carbon dioxide in the blood, as well as the pH.
Treatment:
Treatment depends on the cause and severity of the pulmonary edema. The main goals are to improve breathing and treat the underlying cause.
![]() Oxygen therapy: Administering supplemental oxygen through a mask or nasal cannula.
Oxygen therapy: Administering supplemental oxygen through a mask or nasal cannula.
![]() Medications:
Medications:![]()

![]() Diuretics (water pills): To remove excess fluid from the body. Furosemide (Lasix) is commonly used.
Diuretics (water pills): To remove excess fluid from the body. Furosemide (Lasix) is commonly used.![]()

![]() Morphine: Can reduce shortness of breath and anxiety (used with caution).
Morphine: Can reduce shortness of breath and anxiety (used with caution).![]()

![]() Nitroglycerin: To dilate blood vessels and reduce the heart's workload (if caused by heart problems).
Nitroglycerin: To dilate blood vessels and reduce the heart's workload (if caused by heart problems).![]()

![]() Medications to treat the underlying cause: Such as antibiotics for pneumonia, or medications to improve heart function.
Medications to treat the underlying cause: Such as antibiotics for pneumonia, or medications to improve heart function.
![]() Ventilation support: In severe cases, a ventilator (breathing machine) may be needed to assist or take over breathing.
Ventilation support: In severe cases, a ventilator (breathing machine) may be needed to assist or take over breathing.![]()

![]() CPAP or BiPAP: Non-invasive ventilation using a mask.
CPAP or BiPAP: Non-invasive ventilation using a mask.![]()

![]() Endotracheal intubation and mechanical ventilation: Invasive ventilation.
Endotracheal intubation and mechanical ventilation: Invasive ventilation.
![]() Ultrafiltration: A process to remove excess fluid from the body when diuretics are not effective.
Ultrafiltration: A process to remove excess fluid from the body when diuretics are not effective.
Important Considerations:
![]() Pulmonary edema is a serious condition that requires prompt medical attention. If you experience sudden or severe shortness of breath, especially if you have a history of heart problems, seek emergency medical care immediately.
Pulmonary edema is a serious condition that requires prompt medical attention. If you experience sudden or severe shortness of breath, especially if you have a history of heart problems, seek emergency medical care immediately.
![]() Early diagnosis and treatment are crucial to improve outcomes and prevent complications.
Early diagnosis and treatment are crucial to improve outcomes and prevent complications.
![]() Management of chronic pulmonary edema focuses on managing the underlying cause (e.g., heart failure) and preventing fluid buildup. This often involves lifestyle modifications such as limiting salt intake, monitoring fluid intake, and taking medications as prescribed.
Management of chronic pulmonary edema focuses on managing the underlying cause (e.g., heart failure) and preventing fluid buildup. This often involves lifestyle modifications such as limiting salt intake, monitoring fluid intake, and taking medications as prescribed.
![]() Prevention strategies depend on the underlying cause. For example, managing heart conditions, avoiding smoking, and gradually acclimating to high altitudes can help reduce the risk of pulmonary edema.
Prevention strategies depend on the underlying cause. For example, managing heart conditions, avoiding smoking, and gradually acclimating to high altitudes can help reduce the risk of pulmonary edema.
This information is for general knowledge and does not substitute professional medical advice. Always consult with a qualified healthcare provider for diagnosis and treatment.