Reflux (GERD)
Published: 18 Jun 2025
ICD9: 530.81 ICD10: K21.9 ICD11: DA22
GERD, or Gastroesophageal Reflux Disease, is a chronic digestive disease that occurs when stomach acid or, occasionally, stomach content flows back into the esophagus (the tube that connects your mouth to your stomach).
This backwash (reflux) can irritate the lining of your esophagus.
Here's a breakdown of what that means and its key aspects:
What's happening:
![]() Esophagus: The food tube that connects your mouth to your stomach.
Esophagus: The food tube that connects your mouth to your stomach.
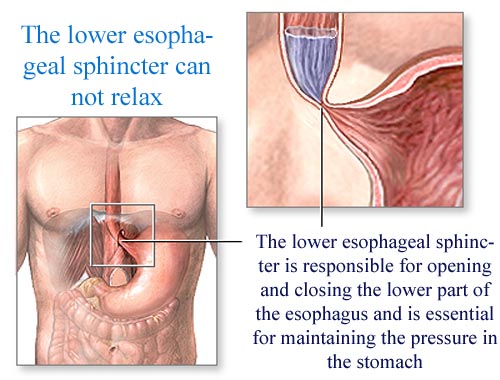
![]() Lower Esophageal Sphincter (LES): A ring of muscle at the bottom of your esophagus that acts like a valve. It's supposed to open to let food into your stomach and then close tightly to prevent stomach acid from backing up.
Lower Esophageal Sphincter (LES): A ring of muscle at the bottom of your esophagus that acts like a valve. It's supposed to open to let food into your stomach and then close tightly to prevent stomach acid from backing up.
![]() Reflux: When the LES doesn't close properly, or opens too often, stomach acid and contents can flow back up into the esophagus. This is called reflux.
Reflux: When the LES doesn't close properly, or opens too often, stomach acid and contents can flow back up into the esophagus. This is called reflux.
![]() Irritation & Inflammation: The stomach acid is very strong and irritates the sensitive lining of the esophagus, causing inflammation and pain.
Irritation & Inflammation: The stomach acid is very strong and irritates the sensitive lining of the esophagus, causing inflammation and pain.
Key aspects and symptoms:
![]() Heartburn: A burning sensation in the chest, often felt after eating, that may be worse at night. This is the most common symptom.
Heartburn: A burning sensation in the chest, often felt after eating, that may be worse at night. This is the most common symptom.
![]() Regurgitation: The sensation of food or sour liquid coming up into your throat or mouth.
Regurgitation: The sensation of food or sour liquid coming up into your throat or mouth.
![]() Other symptoms:
Other symptoms:![]()

![]() Chest pain
Chest pain![]()

![]() Difficulty swallowing (dysphagia)
Difficulty swallowing (dysphagia)![]()

![]() Dry cough
Dry cough![]()

![]() Hoarseness
Hoarseness![]()

![]() Sore throat
Sore throat![]()

![]() Feeling like you have a lump in your throat
Feeling like you have a lump in your throat![]()

![]() New or worsening asthma
New or worsening asthma![]()

![]() Sleep disturbances
Sleep disturbances![]()

![]() Dental erosion
Dental erosion
Causes and Risk Factors:
![]() Hiatal Hernia: When part of the stomach bulges through the diaphragm (the muscle that separates the chest and abdomen), it can weaken the LES.
Hiatal Hernia: When part of the stomach bulges through the diaphragm (the muscle that separates the chest and abdomen), it can weaken the LES.
![]() Obesity: Excess weight can increase pressure on the stomach.
Obesity: Excess weight can increase pressure on the stomach.
![]() Pregnancy: Hormonal changes and increased pressure on the abdomen can contribute to GERD.
Pregnancy: Hormonal changes and increased pressure on the abdomen can contribute to GERD.
![]() Smoking: Can weaken the LES.
Smoking: Can weaken the LES.
![]() Certain Foods: Fatty foods, spicy foods, chocolate, caffeine, alcohol, mint, and carbonated beverages can trigger reflux in some people.
Certain Foods: Fatty foods, spicy foods, chocolate, caffeine, alcohol, mint, and carbonated beverages can trigger reflux in some people.
![]() Delayed Stomach Emptying: If your stomach empties slowly, there's more pressure, increasing the likelihood of reflux.
Delayed Stomach Emptying: If your stomach empties slowly, there's more pressure, increasing the likelihood of reflux.
![]() Certain Medications: Some medications, such as aspirin, ibuprofen, and certain blood pressure medications, can irritate the esophagus or relax the LES.
Certain Medications: Some medications, such as aspirin, ibuprofen, and certain blood pressure medications, can irritate the esophagus or relax the LES.
![]() Connective Tissue Disorders: Such as scleroderma, can affect the LES.
Connective Tissue Disorders: Such as scleroderma, can affect the LES.
Why is it important to treat GERD?
While occasional heartburn is common, chronic GERD can lead to more serious complications if left untreated:
![]() Esophagitis: Inflammation of the esophagus, which can cause pain and difficulty swallowing.
Esophagitis: Inflammation of the esophagus, which can cause pain and difficulty swallowing.
![]() Esophageal Stricture: Narrowing of the esophagus due to scar tissue from chronic inflammation, leading to difficulty swallowing.
Esophageal Stricture: Narrowing of the esophagus due to scar tissue from chronic inflammation, leading to difficulty swallowing.
![]() Barrett's Esophagus: A change in the lining of the esophagus that increases the risk of esophageal cancer.
Barrett's Esophagus: A change in the lining of the esophagus that increases the risk of esophageal cancer.
![]() Esophageal Cancer: A serious complication that can develop from Barrett's esophagus.
Esophageal Cancer: A serious complication that can develop from Barrett's esophagus.
![]() Respiratory problems: Including asthma, chronic cough, and laryngitis.
Respiratory problems: Including asthma, chronic cough, and laryngitis.
Diagnosis:
A doctor can usually diagnose GERD based on your symptoms and a physical exam. Further testing may be needed to confirm the diagnosis or check for complications. These tests may include:
![]() Upper Endoscopy: A thin, flexible tube with a camera is inserted into the esophagus to visualize the lining.
Upper Endoscopy: A thin, flexible tube with a camera is inserted into the esophagus to visualize the lining.
![]() Esophageal pH Monitoring: Measures the amount of acid in the esophagus over a period of time (usually 24 hours).
Esophageal pH Monitoring: Measures the amount of acid in the esophagus over a period of time (usually 24 hours).
![]() Esophageal Manometry: Measures the pressure in the esophagus and LES.
Esophageal Manometry: Measures the pressure in the esophagus and LES.
![]() Barium Swallow: X-rays are taken after you drink a barium solution, which coats the esophagus and makes it easier to see.
Barium Swallow: X-rays are taken after you drink a barium solution, which coats the esophagus and makes it easier to see.
Treatment:
Treatment for GERD typically involves a combination of lifestyle changes, medications, and, in some cases, surgery.
![]() Lifestyle Changes:
Lifestyle Changes:![]()

![]() Dietary modifications: Avoiding trigger foods, eating smaller meals, and not eating close to bedtime.
Dietary modifications: Avoiding trigger foods, eating smaller meals, and not eating close to bedtime.![]()

![]() Weight loss: If overweight or obese.
Weight loss: If overweight or obese.![]()

![]() Elevating the head of the bed: Using blocks or a wedge pillow to raise the head of the bed 6-8 inches.
Elevating the head of the bed: Using blocks or a wedge pillow to raise the head of the bed 6-8 inches.![]()

![]() Quitting smoking:
Quitting smoking:![]()

![]() Avoiding alcohol:
Avoiding alcohol:![]()

![]() Not lying down after eating:
Not lying down after eating:
![]() Medications:
Medications:![]()

![]() Antacids: Provide quick, short-term relief by neutralizing stomach acid.
Antacids: Provide quick, short-term relief by neutralizing stomach acid.![]()

![]() H2 Blockers: Reduce acid production in the stomach.
H2 Blockers: Reduce acid production in the stomach.![]()

![]() Proton Pump Inhibitors (PPIs): More powerful than H2 blockers and block acid production.
Proton Pump Inhibitors (PPIs): More powerful than H2 blockers and block acid production.![]()

![]() Prokinetics: Help the stomach empty faster.
Prokinetics: Help the stomach empty faster.
![]() Surgery: In some cases, surgery may be needed to strengthen the LES. The most common surgery for GERD is called fundoplication.
Surgery: In some cases, surgery may be needed to strengthen the LES. The most common surgery for GERD is called fundoplication.
In summary, GERD is a common and often treatable condition. If you experience frequent heartburn or other symptoms of GERD, it's important to see a doctor to get a proper diagnosis and treatment plan. They can help you manage your symptoms and prevent complications.