Renal ischemia
Published: 18 Jun 2025
ICD9: 593.81 ICD10: N28.0 ICD11: GB90.3
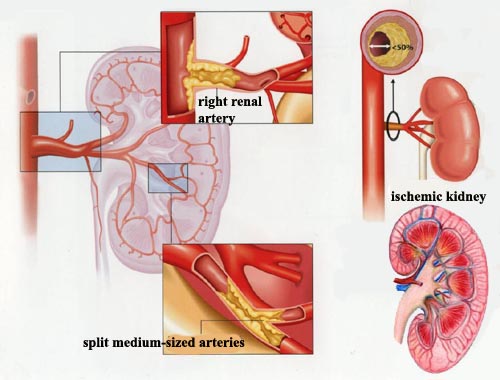
Renal ischemia refers to a condition where the kidneys don't receive enough blood supply.
This lack of blood flow deprives the kidney cells of oxygen and nutrients, leading to potential damage and dysfunction.
Here's a breakdown:
![]() Renal: Relating to the kidneys.
Renal: Relating to the kidneys.
![]() Ischemia: A condition in which the blood flow (and thus oxygen and nutrients) is restricted or reduced in a part of the body.
Ischemia: A condition in which the blood flow (and thus oxygen and nutrients) is restricted or reduced in a part of the body.
Causes of Renal Ischemia:
Renal ischemia can arise from various factors that affect blood flow to the kidneys, including:
![]() Arterial blockage:
Arterial blockage:![]()

![]() Renal artery stenosis: Narrowing of one or both renal arteries. This is often caused by atherosclerosis (plaque buildup) or fibromuscular dysplasia (abnormal cell growth in the artery wall).
Renal artery stenosis: Narrowing of one or both renal arteries. This is often caused by atherosclerosis (plaque buildup) or fibromuscular dysplasia (abnormal cell growth in the artery wall).![]()

![]() Renal artery thrombosis/embolism: A blood clot (thrombus) forming in the renal artery or a clot (embolus) traveling from elsewhere in the body and lodging in the renal artery.
Renal artery thrombosis/embolism: A blood clot (thrombus) forming in the renal artery or a clot (embolus) traveling from elsewhere in the body and lodging in the renal artery.
![]() Hypotension (Low Blood Pressure): Significantly low blood pressure, whether due to severe dehydration, shock, heart failure, or certain medications, can reduce blood flow to the kidneys.
Hypotension (Low Blood Pressure): Significantly low blood pressure, whether due to severe dehydration, shock, heart failure, or certain medications, can reduce blood flow to the kidneys.
![]() Surgery or procedures: Procedures involving the aorta or renal arteries can sometimes cause ischemia.
Surgery or procedures: Procedures involving the aorta or renal arteries can sometimes cause ischemia.
![]() Vasoconstriction: Certain medications or conditions can cause the blood vessels in the kidneys to constrict (narrow), reducing blood flow.
Vasoconstriction: Certain medications or conditions can cause the blood vessels in the kidneys to constrict (narrow), reducing blood flow.
![]() Kidney transplant complications: Ischemia can occur after a kidney transplant if there are problems with the blood supply to the new kidney.
Kidney transplant complications: Ischemia can occur after a kidney transplant if there are problems with the blood supply to the new kidney.
![]() Other conditions: Rarely, certain conditions like vasculitis (inflammation of blood vessels) or aortic dissection can lead to renal ischemia.
Other conditions: Rarely, certain conditions like vasculitis (inflammation of blood vessels) or aortic dissection can lead to renal ischemia.
Symptoms of Renal Ischemia:
The symptoms of renal ischemia can vary depending on the severity and duration of the reduced blood flow. Acute (sudden) ischemia may cause more noticeable symptoms than chronic (gradual) ischemia.
![]() Acute Renal Ischemia:
Acute Renal Ischemia:![]()

![]() Sudden, severe flank pain (pain in the side of the body, between the ribs and hip).
Sudden, severe flank pain (pain in the side of the body, between the ribs and hip).![]()

![]() Nausea and vomiting.
Nausea and vomiting.![]()

![]() Hematuria (blood in the urine).
Hematuria (blood in the urine).![]()

![]() Decreased urine output (oliguria).
Decreased urine output (oliguria).![]()

![]() Elevated blood pressure (hypertension).
Elevated blood pressure (hypertension).![]()

![]() Acute kidney injury (sudden loss of kidney function).
Acute kidney injury (sudden loss of kidney function).
![]() Chronic Renal Ischemia:
Chronic Renal Ischemia:![]()

![]() Hypertension (often difficult to control).
Hypertension (often difficult to control).![]()

![]() Gradual decline in kidney function.
Gradual decline in kidney function.![]()

![]() Fluid retention (edema, swelling).
Fluid retention (edema, swelling).![]()

![]() Fatigue.
Fatigue.![]()

![]() Loss of appetite.
Loss of appetite.![]()

![]() Headaches.
Headaches.
Diagnosis of Renal Ischemia:
Doctors use several methods to diagnose renal ischemia:
![]() Physical examination and medical history: The doctor will ask about symptoms, medical history, and risk factors.
Physical examination and medical history: The doctor will ask about symptoms, medical history, and risk factors.
![]() Blood tests: To assess kidney function (creatinine, BUN), electrolyte levels, and complete blood count.
Blood tests: To assess kidney function (creatinine, BUN), electrolyte levels, and complete blood count.
![]() Urine tests: To check for blood, protein, and other abnormalities.
Urine tests: To check for blood, protein, and other abnormalities.
![]() Renal artery Doppler ultrasound: Uses sound waves to assess blood flow in the renal arteries.
Renal artery Doppler ultrasound: Uses sound waves to assess blood flow in the renal arteries.
![]() Computed tomography angiography (CTA) or magnetic resonance angiography (MRA): Imaging tests that provide detailed pictures of the renal arteries. CTA uses X-rays and contrast dye, while MRA uses magnetic fields and radio waves.
Computed tomography angiography (CTA) or magnetic resonance angiography (MRA): Imaging tests that provide detailed pictures of the renal arteries. CTA uses X-rays and contrast dye, while MRA uses magnetic fields and radio waves.
![]() Renal arteriography (angiogram): An invasive procedure where a catheter is inserted into an artery (usually in the groin) and guided to the renal arteries. Contrast dye is injected, and X-rays are taken to visualize the arteries. This is often used when intervention is planned.
Renal arteriography (angiogram): An invasive procedure where a catheter is inserted into an artery (usually in the groin) and guided to the renal arteries. Contrast dye is injected, and X-rays are taken to visualize the arteries. This is often used when intervention is planned.
![]() Renal scan: Uses radioactive tracers to evaluate kidney function and blood flow.
Renal scan: Uses radioactive tracers to evaluate kidney function and blood flow.
Treatment of Renal Ischemia:
Treatment depends on the cause, severity, and duration of the ischemia.
![]() Medical management:
Medical management:![]()

![]() Blood pressure control: Medications to lower blood pressure are crucial, especially in chronic ischemia. ACE inhibitors or ARBs are often used, but should be used with caution if bilateral renal artery stenosis is suspected or present.
Blood pressure control: Medications to lower blood pressure are crucial, especially in chronic ischemia. ACE inhibitors or ARBs are often used, but should be used with caution if bilateral renal artery stenosis is suspected or present.![]()

![]() Cholesterol-lowering medications (statins): If atherosclerosis is a cause.
Cholesterol-lowering medications (statins): If atherosclerosis is a cause.![]()

![]() Anticoagulants or antiplatelet medications: To prevent blood clots (e.g., aspirin, clopidogrel, warfarin).
Anticoagulants or antiplatelet medications: To prevent blood clots (e.g., aspirin, clopidogrel, warfarin).![]()

![]() Intravenous fluids: To maintain adequate blood volume, especially in cases of hypotension.
Intravenous fluids: To maintain adequate blood volume, especially in cases of hypotension.
![]() Surgical or interventional procedures:
Surgical or interventional procedures:![]()

![]() Angioplasty and stenting: A balloon catheter is inserted into the narrowed renal artery and inflated to widen it. A stent (a small mesh tube) is then placed to keep the artery open.
Angioplasty and stenting: A balloon catheter is inserted into the narrowed renal artery and inflated to widen it. A stent (a small mesh tube) is then placed to keep the artery open.![]()

![]() Renal artery bypass surgery: A surgical procedure to create a new route for blood flow around the blocked renal artery.
Renal artery bypass surgery: A surgical procedure to create a new route for blood flow around the blocked renal artery.![]()

![]() Thrombolysis or embolectomy: To dissolve or remove blood clots blocking the renal artery. This is usually done in cases of acute ischemia.
Thrombolysis or embolectomy: To dissolve or remove blood clots blocking the renal artery. This is usually done in cases of acute ischemia.
![]() Dialysis: May be necessary if kidney function is severely impaired.
Dialysis: May be necessary if kidney function is severely impaired.
![]() Kidney transplant: In cases of end-stage renal disease due to chronic ischemia.
Kidney transplant: In cases of end-stage renal disease due to chronic ischemia.
Complications of Renal Ischemia:
![]() Acute kidney injury (AKI): Sudden loss of kidney function.
Acute kidney injury (AKI): Sudden loss of kidney function.
![]() Chronic kidney disease (CKD): Progressive loss of kidney function over time.
Chronic kidney disease (CKD): Progressive loss of kidney function over time.
![]() End-stage renal disease (ESRD): Complete kidney failure, requiring dialysis or kidney transplant.
End-stage renal disease (ESRD): Complete kidney failure, requiring dialysis or kidney transplant.
![]() Hypertension: High blood pressure that is difficult to control.
Hypertension: High blood pressure that is difficult to control.
![]() Heart failure: Due to fluid retention and increased blood pressure.
Heart failure: Due to fluid retention and increased blood pressure.
![]() Stroke or heart attack: If the underlying cause is atherosclerosis.
Stroke or heart attack: If the underlying cause is atherosclerosis.
In summary, renal ischemia is a serious condition that can lead to kidney damage and failure. Prompt diagnosis and treatment are crucial to preserve kidney function and prevent complications. If you experience symptoms suggestive of renal ischemia, it's important to seek medical attention immediately.