Sickle Cell Disease (Sickle cell anemia)
Published: 18 Jun 2025
ICD9: 282.60 ICD10: D57.1 ICD11: 3A51
Sickle cell disease (SCD), also known as sickle cell anemia, is a group of inherited red blood cell disorders.
It affects the structure of hemoglobin, the protein in red blood cells that carries oxygen throughout the body.
Here's a breakdown:
![]() Normal Red Blood Cells: Red blood cells are normally round and flexible, allowing them to easily move through small blood vessels.
Normal Red Blood Cells: Red blood cells are normally round and flexible, allowing them to easily move through small blood vessels.
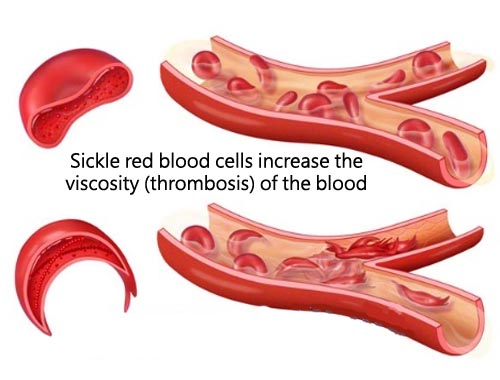
![]() Sickle-Shaped Red Blood Cells: In sickle cell disease, the abnormal hemoglobin causes red blood cells to become rigid and sickle-shaped (like a crescent moon).
Sickle-Shaped Red Blood Cells: In sickle cell disease, the abnormal hemoglobin causes red blood cells to become rigid and sickle-shaped (like a crescent moon).
![]() Cause: SCD is caused by a mutation in the gene that tells your body to make hemoglobin. People with SCD inherit two copies of the sickle cell gene, one from each parent.
Cause: SCD is caused by a mutation in the gene that tells your body to make hemoglobin. People with SCD inherit two copies of the sickle cell gene, one from each parent.
![]() Consequences of Sickle-Shaped Cells:
Consequences of Sickle-Shaped Cells:![]()

![]() Blocked Blood Flow: These sickle cells are sticky and can get stuck in small blood vessels, blocking blood flow.
Blocked Blood Flow: These sickle cells are sticky and can get stuck in small blood vessels, blocking blood flow.![]()

![]() Pain Crises: This blockage leads to episodes of severe pain, known as pain crises, which can occur in any part of the body.
Pain Crises: This blockage leads to episodes of severe pain, known as pain crises, which can occur in any part of the body.![]()

![]() Anemia: Sickle cells break down more quickly than normal red blood cells, leading to a chronic shortage of red blood cells (anemia). Normal red blood cells live about 120 days, while sickle cells typically only live about 10 to 20 days.
Anemia: Sickle cells break down more quickly than normal red blood cells, leading to a chronic shortage of red blood cells (anemia). Normal red blood cells live about 120 days, while sickle cells typically only live about 10 to 20 days.![]()

![]() Organ Damage: The lack of oxygen due to blocked blood flow can damage organs over time, leading to serious complications.
Organ Damage: The lack of oxygen due to blocked blood flow can damage organs over time, leading to serious complications.
![]() Signs and Symptoms: Signs and symptoms of sickle cell disease usually appear in infancy or early childhood. They vary from person to person and can change over time. Common signs and symptoms include:
Signs and Symptoms: Signs and symptoms of sickle cell disease usually appear in infancy or early childhood. They vary from person to person and can change over time. Common signs and symptoms include:![]()

![]() Anemia: Fatigue, paleness, and shortness of breath.
Anemia: Fatigue, paleness, and shortness of breath.![]()

![]() Pain Crises: Episodes of intense pain.
Pain Crises: Episodes of intense pain.![]()

![]() Swelling of Hands and Feet: Due to blocked blood flow.
Swelling of Hands and Feet: Due to blocked blood flow.![]()

![]() Frequent Infections: Sickle cell disease can damage the spleen, which helps fight infection.
Frequent Infections: Sickle cell disease can damage the spleen, which helps fight infection.![]()

![]() Delayed Growth or Puberty:
Delayed Growth or Puberty:![]()

![]() Vision Problems: Blockage of blood vessels in the eye can cause vision problems.
Vision Problems: Blockage of blood vessels in the eye can cause vision problems.
![]() Complications: SCD can lead to various complications, including:
Complications: SCD can lead to various complications, including:![]()

![]() Stroke: Blocked blood flow to the brain.
Stroke: Blocked blood flow to the brain.![]()

![]() Acute Chest Syndrome: A lung infection or blockage of blood vessels in the lungs.
Acute Chest Syndrome: A lung infection or blockage of blood vessels in the lungs.![]()

![]() Pulmonary Hypertension: High blood pressure in the lungs.
Pulmonary Hypertension: High blood pressure in the lungs.![]()

![]() Organ Damage: Kidneys, liver, spleen, and other organs can be damaged.
Organ Damage: Kidneys, liver, spleen, and other organs can be damaged.![]()

![]() Leg Ulcers: Open sores on the legs.
Leg Ulcers: Open sores on the legs.![]()

![]() Gallstones:
Gallstones:
![]() Diagnosis: SCD is typically diagnosed through a blood test called hemoglobin electrophoresis. Newborn screening programs often include testing for sickle cell disease.
Diagnosis: SCD is typically diagnosed through a blood test called hemoglobin electrophoresis. Newborn screening programs often include testing for sickle cell disease.
![]() Treatment: Treatment for sickle cell disease focuses on managing symptoms and preventing complications. Treatments may include:
Treatment: Treatment for sickle cell disease focuses on managing symptoms and preventing complications. Treatments may include:![]()

![]() Pain medication: To relieve pain crises.
Pain medication: To relieve pain crises.![]()

![]() Blood transfusions: To treat anemia and prevent strokes.
Blood transfusions: To treat anemia and prevent strokes.![]()

![]() Hydroxyurea: A medication that can reduce the frequency of pain crises.
Hydroxyurea: A medication that can reduce the frequency of pain crises.![]()

![]() L-glutamine oral powder (Endari): Another medication that helps to reduce acute complications.
L-glutamine oral powder (Endari): Another medication that helps to reduce acute complications.![]()

![]() Crizanlizumab-tmca (Adakveo): A monoclonal antibody that can prevent pain crises by targeting P-selectin.
Crizanlizumab-tmca (Adakveo): A monoclonal antibody that can prevent pain crises by targeting P-selectin.![]()

![]() Voxelotor (Oxbryta): An oral medication that works by binding to hemoglobin to increase hemoglobin's affinity for oxygen. This helps to prevent sickling of red blood cells.
Voxelotor (Oxbryta): An oral medication that works by binding to hemoglobin to increase hemoglobin's affinity for oxygen. This helps to prevent sickling of red blood cells.![]()

![]() Bone marrow transplant (stem cell transplant): A potentially curative treatment, but it carries significant risks.
Bone marrow transplant (stem cell transplant): A potentially curative treatment, but it carries significant risks.![]()

![]() Gene therapy: A promising new area of research that aims to correct the genetic defect that causes sickle cell disease.
Gene therapy: A promising new area of research that aims to correct the genetic defect that causes sickle cell disease.
![]() Inheritance: SCD is an autosomal recessive genetic disorder. This means that a person must inherit two copies of the mutated gene (one from each parent) to have the disease. If a person inherits only one copy of the gene, they are a carrier of the sickle cell trait. Carriers usually don't have symptoms but can pass the gene on to their children. If both parents are carriers, there is a 25% chance with each pregnancy that the child will have SCD, a 50% chance that the child will be a carrier, and a 25% chance that the child will not have the gene at all.
Inheritance: SCD is an autosomal recessive genetic disorder. This means that a person must inherit two copies of the mutated gene (one from each parent) to have the disease. If a person inherits only one copy of the gene, they are a carrier of the sickle cell trait. Carriers usually don't have symptoms but can pass the gene on to their children. If both parents are carriers, there is a 25% chance with each pregnancy that the child will have SCD, a 50% chance that the child will be a carrier, and a 25% chance that the child will not have the gene at all.
![]() Prevalence: SCD is most common in people of African descent, but it also affects people of Hispanic, Mediterranean, Middle Eastern, and South Asian ancestry.
Prevalence: SCD is most common in people of African descent, but it also affects people of Hispanic, Mediterranean, Middle Eastern, and South Asian ancestry.
It's important to consult with a healthcare professional for accurate diagnosis and treatment of sickle cell disease. They can provide the most up-to-date information and personalized care.