Splenic, hepatic, or peritoneal Hematoma (Hematoma in abdomen)
Published: 18 Jun 2025
ICD9: 459.0 ICD10: R58 ICD11: NB9Y
A splenic, hepatic, or peritoneal hematoma (hematoma in the abdomen) is a collection of blood outside of blood vessels, within the abdomen, involving the spleen (splenic), liver (hepatic), or peritoneum (the lining of the abdominal cavity).
Let's break down each component:
![]() Hematoma: This is simply a collection of blood outside of blood vessels, often caused by injury or trauma to the body. It's essentially a bruise, but in this case, it's happening inside the abdomen.
Hematoma: This is simply a collection of blood outside of blood vessels, often caused by injury or trauma to the body. It's essentially a bruise, but in this case, it's happening inside the abdomen.
![]() Splenic Hematoma: This is a hematoma specifically located within or around the spleen. The spleen is an organ located in the upper left abdomen that filters blood, stores blood cells, and helps fight infection.
Splenic Hematoma: This is a hematoma specifically located within or around the spleen. The spleen is an organ located in the upper left abdomen that filters blood, stores blood cells, and helps fight infection.
![]() Hepatic Hematoma: This is a hematoma specifically located within or around the liver. The liver is a large organ located in the upper right abdomen responsible for many vital functions, including filtering blood, producing bile, and metabolizing drugs.
Hepatic Hematoma: This is a hematoma specifically located within or around the liver. The liver is a large organ located in the upper right abdomen responsible for many vital functions, including filtering blood, producing bile, and metabolizing drugs.
![]() Peritoneal Hematoma: This is a hematoma within the peritoneal cavity, the space between the peritoneum (the membrane lining the abdominal wall) and the abdominal organs. Blood can collect anywhere within this space.
Peritoneal Hematoma: This is a hematoma within the peritoneal cavity, the space between the peritoneum (the membrane lining the abdominal wall) and the abdominal organs. Blood can collect anywhere within this space.
Causes:
![]() Trauma: This is the most common cause. Car accidents, falls, or direct blows to the abdomen can rupture blood vessels in the spleen, liver, or peritoneal lining, leading to hematoma formation.
Trauma: This is the most common cause. Car accidents, falls, or direct blows to the abdomen can rupture blood vessels in the spleen, liver, or peritoneal lining, leading to hematoma formation.
![]() Surgery: Abdominal surgery can sometimes damage blood vessels, resulting in a post-operative hematoma.
Surgery: Abdominal surgery can sometimes damage blood vessels, resulting in a post-operative hematoma.
![]() Medical Procedures: Procedures like biopsies or drain placements can occasionally cause bleeding.
Medical Procedures: Procedures like biopsies or drain placements can occasionally cause bleeding.
![]() Underlying Medical Conditions: Rarely, conditions that affect blood clotting (e.g., hemophilia, thrombocytopenia) or liver disease can increase the risk of spontaneous hematomas.
Underlying Medical Conditions: Rarely, conditions that affect blood clotting (e.g., hemophilia, thrombocytopenia) or liver disease can increase the risk of spontaneous hematomas.
![]() Spontaneous Rupture: In rare cases, a splenic or hepatic hematoma can occur spontaneously, often due to an underlying weakened blood vessel or tumor.
Spontaneous Rupture: In rare cases, a splenic or hepatic hematoma can occur spontaneously, often due to an underlying weakened blood vessel or tumor.
Symptoms:
Symptoms can vary widely depending on the size and location of the hematoma, the speed of blood loss, and the overall health of the patient. Common symptoms may include:
![]() Abdominal Pain: The location and intensity of pain can vary. It might be sharp, dull, constant, or intermittent.
Abdominal Pain: The location and intensity of pain can vary. It might be sharp, dull, constant, or intermittent.
![]() Abdominal Tenderness: The abdomen may be painful to the touch.
Abdominal Tenderness: The abdomen may be painful to the touch.
![]() Abdominal Distention: The abdomen may become swollen or bloated due to the accumulation of blood.
Abdominal Distention: The abdomen may become swollen or bloated due to the accumulation of blood.
![]() Bruising: External bruising may be present on the abdomen, but it's not always the case, especially with internal hematomas.
Bruising: External bruising may be present on the abdomen, but it's not always the case, especially with internal hematomas.
![]() Lightheadedness or Dizziness: This can occur if there is significant blood loss.
Lightheadedness or Dizziness: This can occur if there is significant blood loss.
![]() Rapid Heart Rate (Tachycardia): A sign of blood loss.
Rapid Heart Rate (Tachycardia): A sign of blood loss.
![]() Low Blood Pressure (Hypotension): A sign of blood loss.
Low Blood Pressure (Hypotension): A sign of blood loss.
![]() Nausea and Vomiting:
Nausea and Vomiting:
![]() Shoulder Pain (Referred Pain): Irritation of the diaphragm by the blood can sometimes cause pain in the shoulder (especially the left shoulder for a splenic hematoma).
Shoulder Pain (Referred Pain): Irritation of the diaphragm by the blood can sometimes cause pain in the shoulder (especially the left shoulder for a splenic hematoma).
![]() In severe cases, shock: Signs of shock include pale skin, rapid breathing, confusion, and loss of consciousness. This is a medical emergency.
In severe cases, shock: Signs of shock include pale skin, rapid breathing, confusion, and loss of consciousness. This is a medical emergency.
Diagnosis:
![]() Physical Examination: A doctor will examine the abdomen for tenderness, distention, and other signs of injury.
Physical Examination: A doctor will examine the abdomen for tenderness, distention, and other signs of injury.
![]() Imaging Tests:
Imaging Tests:![]()

![]() CT Scan: This is the most common and reliable imaging test for detecting abdominal hematomas.
CT Scan: This is the most common and reliable imaging test for detecting abdominal hematomas.![]()

![]() Ultrasound: Ultrasound can sometimes be used, especially in emergency situations, but it may not be as detailed as a CT scan.
Ultrasound: Ultrasound can sometimes be used, especially in emergency situations, but it may not be as detailed as a CT scan.![]()

![]() MRI: Less commonly used, but can be helpful in certain situations.
MRI: Less commonly used, but can be helpful in certain situations.
![]() Blood Tests: Blood tests can help assess the patient's overall health, including blood count (to check for blood loss) and clotting factors.
Blood Tests: Blood tests can help assess the patient's overall health, including blood count (to check for blood loss) and clotting factors.
Treatment:
Treatment depends on the size and stability of the hematoma, the patient's overall condition, and whether there are any other injuries.
![]() Observation: Small, stable hematomas may be managed with observation, bed rest, and pain medication. Serial imaging (repeat CT scans) is done to monitor the hematoma's size.
Observation: Small, stable hematomas may be managed with observation, bed rest, and pain medication. Serial imaging (repeat CT scans) is done to monitor the hematoma's size.
![]() Blood Transfusion: If there is significant blood loss, blood transfusions may be necessary.
Blood Transfusion: If there is significant blood loss, blood transfusions may be necessary.
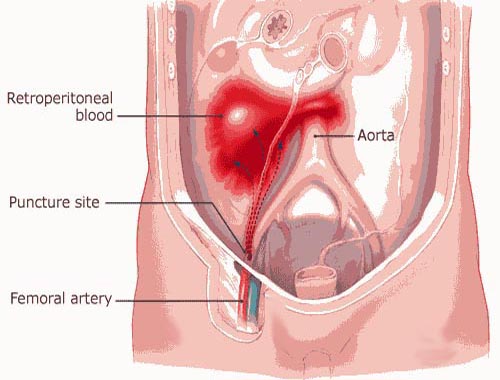
![]() Angioembolization: This is a minimally invasive procedure where a catheter is inserted into a blood vessel to block the bleeding vessel supplying the hematoma.
Angioembolization: This is a minimally invasive procedure where a catheter is inserted into a blood vessel to block the bleeding vessel supplying the hematoma.
![]() Surgery: Surgery may be required for large, expanding, or unstable hematomas, or if there are other injuries that need to be addressed. The goal of surgery is to stop the bleeding and remove the hematoma. Splenectomy (removal of the spleen) or liver resection (removal of part of the liver) may be necessary in severe cases.
Surgery: Surgery may be required for large, expanding, or unstable hematomas, or if there are other injuries that need to be addressed. The goal of surgery is to stop the bleeding and remove the hematoma. Splenectomy (removal of the spleen) or liver resection (removal of part of the liver) may be necessary in severe cases.
![]() Other Supportive Care: IV fluids, oxygen, and other supportive measures may be necessary to stabilize the patient.
Other Supportive Care: IV fluids, oxygen, and other supportive measures may be necessary to stabilize the patient.
Prognosis:
The prognosis depends on the severity of the injury, the patient's overall health, and the promptness and effectiveness of treatment. Small, stable hematomas often resolve on their own with observation. Larger or unstable hematomas require more aggressive treatment and can have a higher risk of complications.
Important Note: Any suspected abdominal injury or pain should be evaluated by a medical professional immediately. A ruptured spleen or liver can be life-threatening due to massive internal bleeding.