Subdural Hematoma
Published: 18 Jun 2025
ICD9: 432.1 ICD10: I62.00 ICD11: 8B02
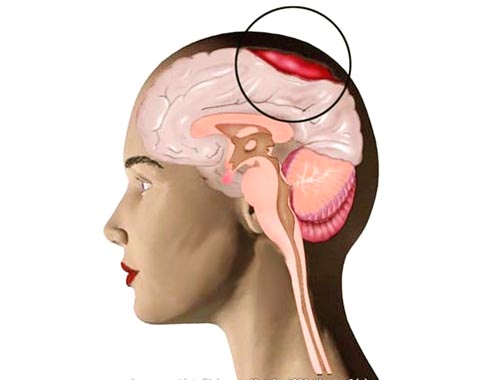
A subdural hematoma (SDH) is a type of hematoma, which is a collection of blood outside the brain.
More specifically, it's a collection of blood that gathers between the dura mater (the outermost layer of the membranes surrounding the brain and spinal cord) and the arachnoid mater (the middle layer).
Here's a breakdown of the key aspects:
![]() Location: Between the dura mater and arachnoid mater. Imagine the brain is like an orange. The peel is the skull, the white pith is the dura mater, and the juicy orange segments are the brain. The subdural hematoma is like blood pooling between the pith and the orange.
Location: Between the dura mater and arachnoid mater. Imagine the brain is like an orange. The peel is the skull, the white pith is the dura mater, and the juicy orange segments are the brain. The subdural hematoma is like blood pooling between the pith and the orange.
![]() Cause: Usually caused by a head injury that tears bridging veins. These are small veins that stretch from the surface of the brain to the dura. Sudden acceleration or deceleration of the head can cause these veins to tear. Less commonly, it can occur spontaneously (without a known injury), especially in people with blood clotting disorders or on blood-thinning medications.
Cause: Usually caused by a head injury that tears bridging veins. These are small veins that stretch from the surface of the brain to the dura. Sudden acceleration or deceleration of the head can cause these veins to tear. Less commonly, it can occur spontaneously (without a known injury), especially in people with blood clotting disorders or on blood-thinning medications.
![]() Types:
Types:![]()

![]() Acute: Occurs soon after a severe head injury. Symptoms develop quickly (within hours). High risk of brain damage or death.
Acute: Occurs soon after a severe head injury. Symptoms develop quickly (within hours). High risk of brain damage or death.![]()

![]() Subacute: Symptoms appear days or weeks after the injury.
Subacute: Symptoms appear days or weeks after the injury.![]()

![]() Chronic: Develops slowly over weeks or months, often after a minor head injury or even without a known injury. More common in older adults, especially those on blood thinners or who have a history of falls.
Chronic: Develops slowly over weeks or months, often after a minor head injury or even without a known injury. More common in older adults, especially those on blood thinners or who have a history of falls.
![]() Symptoms: Symptoms vary depending on the size and rate of bleeding. They can include:
Symptoms: Symptoms vary depending on the size and rate of bleeding. They can include:![]()

![]() Headache
Headache![]()

![]() Confusion
Confusion![]()

![]() Drowsiness
Drowsiness![]()

![]() Slurred speech
Slurred speech![]()

![]() Vision changes
Vision changes![]()

![]() Weakness on one side of the body
Weakness on one side of the body![]()

![]() Seizures
Seizures![]()

![]() Nausea and vomiting
Nausea and vomiting![]()

![]() Changes in behavior
Changes in behavior![]()

![]() Loss of consciousness
Loss of consciousness
In chronic cases, symptoms can be subtle and mistaken for dementia or other age-related cognitive decline.
![]() Diagnosis: Diagnosed with a CT scan or MRI of the head. These imaging techniques can show the location and size of the hematoma.
Diagnosis: Diagnosed with a CT scan or MRI of the head. These imaging techniques can show the location and size of the hematoma.
![]() Treatment: Treatment depends on the size of the hematoma, the severity of symptoms, and the patient's overall health. Options include:
Treatment: Treatment depends on the size of the hematoma, the severity of symptoms, and the patient's overall health. Options include:![]()

![]() Observation: Small hematomas that aren't causing significant symptoms may be monitored closely to see if they resolve on their own.
Observation: Small hematomas that aren't causing significant symptoms may be monitored closely to see if they resolve on their own.![]()

![]() Medications: Medications may be used to control seizures or reduce swelling in the brain. In some cases, medications to reverse the effects of blood thinners might be used.
Medications: Medications may be used to control seizures or reduce swelling in the brain. In some cases, medications to reverse the effects of blood thinners might be used.![]()

![]() Surgery: Larger hematomas or those causing significant symptoms may require surgery to drain the blood. Surgical options include:
Surgery: Larger hematomas or those causing significant symptoms may require surgery to drain the blood. Surgical options include:![]()

![]() Burr hole craniotomy: Small holes are drilled into the skull to drain the blood.
Burr hole craniotomy: Small holes are drilled into the skull to drain the blood.![]()

![]() Craniotomy: A larger section of the skull is removed to allow for better access to the hematoma and to relieve pressure on the brain.
Craniotomy: A larger section of the skull is removed to allow for better access to the hematoma and to relieve pressure on the brain.
![]() Risk Factors:
Risk Factors:![]()

![]() Older age (brain shrinks with age, stretching the bridging veins)
Older age (brain shrinks with age, stretching the bridging veins)![]()

![]() Use of blood-thinning medications (anticoagulants or antiplatelet drugs)
Use of blood-thinning medications (anticoagulants or antiplatelet drugs)![]()

![]() History of falls
History of falls![]()

![]() Alcohol abuse
Alcohol abuse![]()

![]() Brain atrophy (shrinkage)
Brain atrophy (shrinkage)![]()

![]() Head trauma
Head trauma
Important Considerations:
![]() A subdural hematoma is a serious condition that can be life-threatening.
A subdural hematoma is a serious condition that can be life-threatening.
![]() Prompt medical attention is crucial if you suspect someone has a subdural hematoma.
Prompt medical attention is crucial if you suspect someone has a subdural hematoma.
![]() Even seemingly minor head injuries should be evaluated by a doctor, especially if the person is elderly, on blood thinners, or has a history of falls.
Even seemingly minor head injuries should be evaluated by a doctor, especially if the person is elderly, on blood thinners, or has a history of falls.
Disclaimer: This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.