Testicular Cancer
Published: 18 Jun 2025
ICD9: 186.9 ICD10: C62.10 ICD11: 2C80
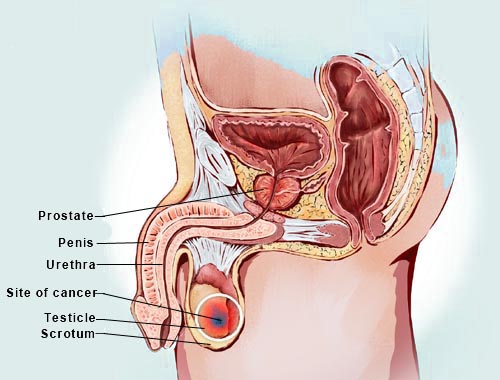
Testicular cancer is a type of cancer that starts in the testicles, which are located inside the scrotum, a loose bag of skin underneath the penis.
The testicles produce male sex hormones and sperm for reproduction.
Here's a breakdown of important aspects:
Key Facts:
![]() Relatively Rare: Testicular cancer is not very common, accounting for only about 1% of cancers in men.
Relatively Rare: Testicular cancer is not very common, accounting for only about 1% of cancers in men.
![]() Highly Treatable: It's one of the most curable cancers, even when it has spread beyond the testicle.
Highly Treatable: It's one of the most curable cancers, even when it has spread beyond the testicle.
![]() Age Group: It most often affects males between the ages of 15 and 45.
Age Group: It most often affects males between the ages of 15 and 45.
![]() Early Detection is Key: Self-examination is crucial for early detection.
Early Detection is Key: Self-examination is crucial for early detection.
Types of Testicular Cancer:
![]() Germ Cell Tumors (GCTs): These account for over 90% of testicular cancers. There are two main subtypes:
Germ Cell Tumors (GCTs): These account for over 90% of testicular cancers. There are two main subtypes:![]()

![]() Seminomas: Tend to grow and spread more slowly.
Seminomas: Tend to grow and spread more slowly.![]()

![]() Nonseminomas: A group of several types (embryonal carcinoma, yolk sac carcinoma, choriocarcinoma, teratoma) that tend to grow and spread more quickly.
Nonseminomas: A group of several types (embryonal carcinoma, yolk sac carcinoma, choriocarcinoma, teratoma) that tend to grow and spread more quickly.
![]() Stromal Tumors: These develop in the supportive and hormone-producing tissues of the testicles. They are less common. Leydig cell tumors and Sertoli cell tumors fall into this category.
Stromal Tumors: These develop in the supportive and hormone-producing tissues of the testicles. They are less common. Leydig cell tumors and Sertoli cell tumors fall into this category.
Risk Factors:
![]() Undescended Testicle (Cryptorchidism): This is the most well-established risk factor.
Undescended Testicle (Cryptorchidism): This is the most well-established risk factor.
![]() Family History: Having a father or brother with testicular cancer increases the risk.
Family History: Having a father or brother with testicular cancer increases the risk.
![]() Personal History: If you've had testicular cancer in one testicle, you're at higher risk of developing it in the other.
Personal History: If you've had testicular cancer in one testicle, you're at higher risk of developing it in the other.
![]() Race: White men are more likely to develop testicular cancer than men of other races.
Race: White men are more likely to develop testicular cancer than men of other races.
![]() Age: Most common in men aged 15 to 45.
Age: Most common in men aged 15 to 45.
![]() HIV infection
HIV infection
![]() Carcinoma in situ (CIS) of the testicle
Carcinoma in situ (CIS) of the testicle
![]() Infertility
Infertility
Symptoms:
![]() A lump or enlargement in either testicle: This is the most common symptom. It may or may not be painful.
A lump or enlargement in either testicle: This is the most common symptom. It may or may not be painful.
![]() A feeling of heaviness in the scrotum.
A feeling of heaviness in the scrotum.
![]() A dull ache in the abdomen or groin.
A dull ache in the abdomen or groin.
![]() Sudden collection of fluid in the scrotum.
Sudden collection of fluid in the scrotum.
![]() Pain or discomfort in a testicle or the scrotum.
Pain or discomfort in a testicle or the scrotum.
![]() Enlargement or tenderness of the breasts (rare).
Enlargement or tenderness of the breasts (rare).
![]() Back pain (if the cancer has spread).
Back pain (if the cancer has spread).
Diagnosis:
![]() Physical Exam: A doctor will examine the testicles and scrotum.
Physical Exam: A doctor will examine the testicles and scrotum.
![]() Ultrasound: This imaging test can help determine if a lump is solid or fluid-filled.
Ultrasound: This imaging test can help determine if a lump is solid or fluid-filled.
![]() Blood Tests: Tumor markers (substances released by cancer cells) can be measured in the blood. Elevated levels of certain markers can suggest testicular cancer.
Blood Tests: Tumor markers (substances released by cancer cells) can be measured in the blood. Elevated levels of certain markers can suggest testicular cancer.
![]() Inguinal Orchiectomy: If cancer is suspected, the entire testicle is surgically removed through an incision in the groin. A biopsy is *not* performed while the testicle is still in the scrotum, as this could spread the cancer. The removed testicle is then examined under a microscope to confirm the diagnosis and determine the type of cancer.
Inguinal Orchiectomy: If cancer is suspected, the entire testicle is surgically removed through an incision in the groin. A biopsy is *not* performed while the testicle is still in the scrotum, as this could spread the cancer. The removed testicle is then examined under a microscope to confirm the diagnosis and determine the type of cancer.
![]() CT Scans: Used to see if the cancer has spread to other parts of the body (staging).
CT Scans: Used to see if the cancer has spread to other parts of the body (staging).
Treatment:
Treatment options depend on the type and stage of the cancer, and the patient's overall health.
![]() Surgery (Orchiectomy): Removal of the affected testicle is the primary treatment.
Surgery (Orchiectomy): Removal of the affected testicle is the primary treatment.
![]() Radiation Therapy: Using high-energy rays to kill cancer cells. Typically used for seminomas.
Radiation Therapy: Using high-energy rays to kill cancer cells. Typically used for seminomas.
![]() Chemotherapy: Using drugs to kill cancer cells throughout the body. Often used for nonseminomas and advanced stages of seminomas.
Chemotherapy: Using drugs to kill cancer cells throughout the body. Often used for nonseminomas and advanced stages of seminomas.
![]() Retroperitoneal Lymph Node Dissection (RPLND): Surgical removal of lymph nodes in the abdomen. This may be necessary if cancer has spread to the lymph nodes. There are nerve-sparing techniques to help maintain fertility.
Retroperitoneal Lymph Node Dissection (RPLND): Surgical removal of lymph nodes in the abdomen. This may be necessary if cancer has spread to the lymph nodes. There are nerve-sparing techniques to help maintain fertility.
Self-Examination:
![]() Testicular self-exams are recommended monthly, especially for men at higher risk.
Testicular self-exams are recommended monthly, especially for men at higher risk.
![]() The best time is after a warm bath or shower when the scrotal skin is relaxed.
The best time is after a warm bath or shower when the scrotal skin is relaxed.
![]() Roll each testicle gently between the thumb and fingers.
Roll each testicle gently between the thumb and fingers.
![]() Feel for any lumps, changes in size or shape, or any areas of hardness.
Feel for any lumps, changes in size or shape, or any areas of hardness.
![]() It's normal for one testicle to be slightly larger than the other, and it's also normal to feel the epididymis (a tube-like structure behind the testicle).
It's normal for one testicle to be slightly larger than the other, and it's also normal to feel the epididymis (a tube-like structure behind the testicle).
![]() If you notice anything unusual, see a doctor promptly.
If you notice anything unusual, see a doctor promptly.
Important Considerations:
![]() Fertility: Treatment for testicular cancer can sometimes affect fertility. Men may want to consider sperm banking before treatment.
Fertility: Treatment for testicular cancer can sometimes affect fertility. Men may want to consider sperm banking before treatment.
![]() Follow-up: Regular follow-up appointments are essential after treatment to monitor for recurrence.
Follow-up: Regular follow-up appointments are essential after treatment to monitor for recurrence.
![]() Prognosis: The prognosis for testicular cancer is generally very good, especially when detected early.
Prognosis: The prognosis for testicular cancer is generally very good, especially when detected early.
Disclaimer: This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.