Thrombophilia (Hypercoagulable state) (Coagulopathy)
Published: 18 Jun 2025
ICD9: 289.81 ICD10: D68.59 ICD11: 3B61
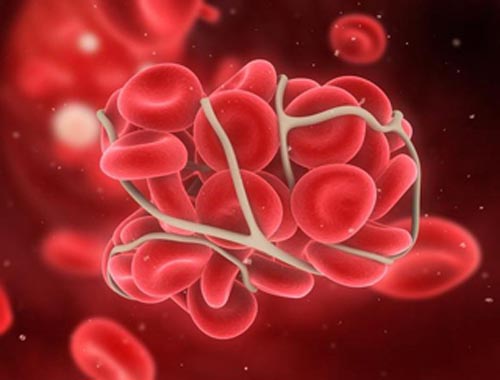
Thrombophilia, also known as a hypercoagulable state or coagulopathy, is a condition in which the blood has an increased tendency to form clots.
This means that individuals with thrombophilia are at a higher risk of developing abnormal blood clots, which can lead to serious health problems.
Here's a breakdown of the terms and a more detailed explanation:
![]() Thrombophilia: This is the most general term and means "love of thrombus" (thrombus = blood clot).
Thrombophilia: This is the most general term and means "love of thrombus" (thrombus = blood clot).
![]() Hypercoagulable State: This term directly describes the condition of having blood that is more prone to clot than normal. "Hyper" means "excessive," and "coagulable" refers to the ability to clot.
Hypercoagulable State: This term directly describes the condition of having blood that is more prone to clot than normal. "Hyper" means "excessive," and "coagulable" refers to the ability to clot.
![]() Coagulopathy: This is a more general term referring to any disorder of blood coagulation (clotting). While thrombophilia is a type of coagulopathy, coagulopathies can also refer to conditions where the blood clots *too little* (e.g., hemophilia). Therefore, it's important to specify "hypercoagulable coagulopathy" or "thrombophilic coagulopathy" for clarity.
Coagulopathy: This is a more general term referring to any disorder of blood coagulation (clotting). While thrombophilia is a type of coagulopathy, coagulopathies can also refer to conditions where the blood clots *too little* (e.g., hemophilia). Therefore, it's important to specify "hypercoagulable coagulopathy" or "thrombophilic coagulopathy" for clarity.
Causes of Thrombophilia:
Thrombophilia can be caused by:
![]() Inherited (Genetic) Factors: These are genetic mutations that affect the proteins involved in blood clotting. Common inherited thrombophilias include:
Inherited (Genetic) Factors: These are genetic mutations that affect the proteins involved in blood clotting. Common inherited thrombophilias include:![]()

![]() Factor V Leiden mutation
Factor V Leiden mutation![]()

![]() Prothrombin G20210A mutation
Prothrombin G20210A mutation![]()

![]() Protein C deficiency
Protein C deficiency![]()

![]() Protein S deficiency
Protein S deficiency![]()

![]() Antithrombin deficiency
Antithrombin deficiency![]()

![]() Elevated Factor VIII levels
Elevated Factor VIII levels
![]() Acquired Factors: These are conditions or factors that develop during a person's lifetime and increase the risk of blood clots. Common acquired thrombophilias include:
Acquired Factors: These are conditions or factors that develop during a person's lifetime and increase the risk of blood clots. Common acquired thrombophilias include:![]()

![]() Antiphospholipid syndrome (APS)
Antiphospholipid syndrome (APS)![]()

![]() Cancer
Cancer![]()

![]() Pregnancy
Pregnancy![]()

![]() Hormone therapy (e.g., birth control pills containing estrogen)
Hormone therapy (e.g., birth control pills containing estrogen)![]()

![]() Prolonged immobility (e.g., after surgery, long plane flights)
Prolonged immobility (e.g., after surgery, long plane flights)![]()

![]() Obesity
Obesity![]()

![]() Smoking
Smoking![]()

![]() Certain medications
Certain medications![]()

![]() Autoimmune diseases (e.g., lupus, rheumatoid arthritis)
Autoimmune diseases (e.g., lupus, rheumatoid arthritis)![]()

![]() Nephrotic syndrome
Nephrotic syndrome![]()

![]() Myeloproliferative neoplasms
Myeloproliferative neoplasms
![]() Mixed Inherited and Acquired Factors: Sometimes, a person may have an inherited tendency to clot, and an acquired factor further increases the risk. For example, a woman with Factor V Leiden mutation taking oral contraceptives has a significantly higher risk of blood clots.
Mixed Inherited and Acquired Factors: Sometimes, a person may have an inherited tendency to clot, and an acquired factor further increases the risk. For example, a woman with Factor V Leiden mutation taking oral contraceptives has a significantly higher risk of blood clots.
Risks and Complications:
The primary risk associated with thrombophilia is an increased risk of developing abnormal blood clots, which can lead to:
![]() Deep Vein Thrombosis (DVT): A blood clot in a deep vein, usually in the leg. Symptoms include pain, swelling, redness, and warmth in the affected leg.
Deep Vein Thrombosis (DVT): A blood clot in a deep vein, usually in the leg. Symptoms include pain, swelling, redness, and warmth in the affected leg.
![]() Pulmonary Embolism (PE): A blood clot that travels to the lungs, blocking blood flow. Symptoms include shortness of breath, chest pain, coughing (possibly with blood), and rapid heart rate. PE can be life-threatening.
Pulmonary Embolism (PE): A blood clot that travels to the lungs, blocking blood flow. Symptoms include shortness of breath, chest pain, coughing (possibly with blood), and rapid heart rate. PE can be life-threatening.
![]() Arterial Thrombosis: Blood clots in arteries, which can lead to stroke, heart attack, or limb ischemia (reduced blood flow to a limb).
Arterial Thrombosis: Blood clots in arteries, which can lead to stroke, heart attack, or limb ischemia (reduced blood flow to a limb).
![]() Recurrent Miscarriage: In pregnant women, thrombophilia can increase the risk of blood clots in the placenta, leading to miscarriage or other pregnancy complications.
Recurrent Miscarriage: In pregnant women, thrombophilia can increase the risk of blood clots in the placenta, leading to miscarriage or other pregnancy complications.
![]() Other complications: Less commonly, blood clots can occur in other locations, such as the brain (cerebral venous thrombosis), abdomen (mesenteric thrombosis), or eyes.
Other complications: Less commonly, blood clots can occur in other locations, such as the brain (cerebral venous thrombosis), abdomen (mesenteric thrombosis), or eyes.
Diagnosis:
Diagnosis usually involves:
![]() Medical History and Physical Exam: The doctor will ask about your personal and family history of blood clots, miscarriages, and other relevant conditions.
Medical History and Physical Exam: The doctor will ask about your personal and family history of blood clots, miscarriages, and other relevant conditions.
![]() Blood Tests: Specific blood tests are performed to identify inherited and acquired thrombophilias. These tests measure the levels and function of various clotting factors and antibodies. Testing is often done when the patient is not actively on anticoagulation.
Blood Tests: Specific blood tests are performed to identify inherited and acquired thrombophilias. These tests measure the levels and function of various clotting factors and antibodies. Testing is often done when the patient is not actively on anticoagulation.
Treatment:
Treatment focuses on preventing and treating blood clots and may include:
![]() Anticoagulant Medications: These medications, also known as blood thinners, help to prevent blood clots from forming or growing. Common anticoagulants include:
Anticoagulant Medications: These medications, also known as blood thinners, help to prevent blood clots from forming or growing. Common anticoagulants include:![]()

![]() Warfarin (Coumadin)
Warfarin (Coumadin)![]()

![]() Heparin (unfractionated heparin, low molecular weight heparin such as enoxaparin/Lovenox)
Heparin (unfractionated heparin, low molecular weight heparin such as enoxaparin/Lovenox)![]()

![]() Direct oral anticoagulants (DOACs) such as rivaroxaban (Xarelto), apixaban (Eliquis), edoxaban (Savaysa), and dabigatran (Pradaxa)
Direct oral anticoagulants (DOACs) such as rivaroxaban (Xarelto), apixaban (Eliquis), edoxaban (Savaysa), and dabigatran (Pradaxa)
![]() Compression Stockings: These can help to improve blood flow in the legs and reduce the risk of DVT.
Compression Stockings: These can help to improve blood flow in the legs and reduce the risk of DVT.
![]() Lifestyle Modifications: Weight loss (if overweight), smoking cessation, and regular exercise can help reduce the risk of blood clots.
Lifestyle Modifications: Weight loss (if overweight), smoking cessation, and regular exercise can help reduce the risk of blood clots.
![]() Monitoring: Regular monitoring of blood clotting levels (e.g., INR for warfarin) is necessary to ensure that the medication is working effectively and safely.
Monitoring: Regular monitoring of blood clotting levels (e.g., INR for warfarin) is necessary to ensure that the medication is working effectively and safely.
Important Considerations:
![]() Not Everyone with Thrombophilia Develops Blood Clots: Many people with thrombophilia never experience a blood clot. The risk of clotting depends on the specific type of thrombophilia, the presence of other risk factors, and individual circumstances.
Not Everyone with Thrombophilia Develops Blood Clots: Many people with thrombophilia never experience a blood clot. The risk of clotting depends on the specific type of thrombophilia, the presence of other risk factors, and individual circumstances.
![]() Management is Individualized: The treatment plan for thrombophilia is tailored to the individual patient, taking into account their specific risk factors, medical history, and the severity of their condition.
Management is Individualized: The treatment plan for thrombophilia is tailored to the individual patient, taking into account their specific risk factors, medical history, and the severity of their condition.
![]() Pregnancy: Pregnant women with thrombophilia require careful monitoring and management to reduce the risk of pregnancy complications.
Pregnancy: Pregnant women with thrombophilia require careful monitoring and management to reduce the risk of pregnancy complications.
![]() Consult a Hematologist: If you suspect you may have thrombophilia or have a family history of blood clots, it's important to consult with a hematologist (a doctor specializing in blood disorders) for proper diagnosis and management.
Consult a Hematologist: If you suspect you may have thrombophilia or have a family history of blood clots, it's important to consult with a hematologist (a doctor specializing in blood disorders) for proper diagnosis and management.
In summary, thrombophilia is a condition that increases the risk of blood clots. It can be caused by inherited or acquired factors, or a combination of both. Proper diagnosis and management are crucial to prevent serious complications. If you have concerns about thrombophilia, it is vital to discuss them with your doctor.